CARE OF UNDER FIVE’S – Under Five’s Clinic, Aims of Under Five Clinics, Objectives of Under Five Clinics, Role of a Nurse in Under Five’s Clinic and Physical Facilities for a Children’s Clinic (CHILD HEALTH NURSING)
UPDATED 2024
THE RIGHTS OF THE CHILD
To meet the special need of the child, the general assembly of the United Nations adopted on 20th November 1959, and the declaration of the Rights of the child. India was a signatory to this declaration
- Right to develop in an atmosphere of affection and security and whenever possible in the care and under the responsibility of his/her parents
- Right to enjoy the benefits of social security including nutrition, housing and medical care
- Right to free education
- Right to full opportunity for play and recreation
- Right to a name and nationality
- Right to special care if handicapped
- Right to be among the first to receive protection and relief in times of disaster
- Right to learn to be a useful member of society and to develop in a healthy and normal manner and in conditions of freedom and dignity
- Right to bring up in a spirit of understanding of brotherhood
- Right to enjoy these rights, regardless of race, color, sex, religion, social and national origin
UNDER FIVE’S CLINIC
The under five’s clinic or well baby clinic’s combines the concepts of prevention, treatment, health supervision, nutritional surveillance, and education into a system of comprehensive health care within the resources available in the country, making use of nonprofessional auxiliaries, thus making the service not only economical but also available to a larger proportion of children in the community. Under five clinics must provide for courteous reception of mother and children, with enthusiasm and zeal on the part of each member of the team
AIMS OF UNDER FIVE CLINICS
Care in illness: the basic philosophy of the under five’s clinic to give nurses effective training and responsibility for handling the child healthcare service. The illness care for children will comprise of diagnosis and treatment, X-ray and laboratory services and referral services
Preventive care: the preventive care given on the basis of immunization, nutritional surveillance, health checkups, oral rehydration, family planning and health education
Growth monitoring: for under five clinic to weigh the child periodically at monthly intervals during the first year, every 2 months during the second year and every 3 months thereafter up to a age of 5 to 6 years. The growth curve will help the health worker to detect early onset of growth failure
OBJECTIVES OF UNDER FIVE CLINICS’
- The prevention of malnutrition, pertussis, tuberculosis, poliomyelitis, diphtheria, tetanus and measles
- The supervision of the health of all children upon the age of five
- The education of parents to promote health and family planning
- The provision of simple treatment for diarrhea, with or without dehydration, pneumonia, skin conditions and other common disorders
ROLE OF A NURSE IN UNDER FIVE’S CLINIC
- Treating minor illness
- Referring the more seriously-ill children
- Instructing about feeding, nutrition and hygiene
- Encouraging child spacing and family planning
- Maintaining the children’s weight cards, e.g. road to good health cards
- Being alert in every conditions so that the effectiveness of the service can be improved
PHYSICAL FACILITIES FOR A CHILDREN’S CLINIC
- Outside compound: playground for children waiting to be served including swings slides and sand box are needed. These facilities may be provided by the community volunteer group or by the health committee
- Waiting room should include a reception table and the record. The area should include child health posters, display exhibits and play are for the children
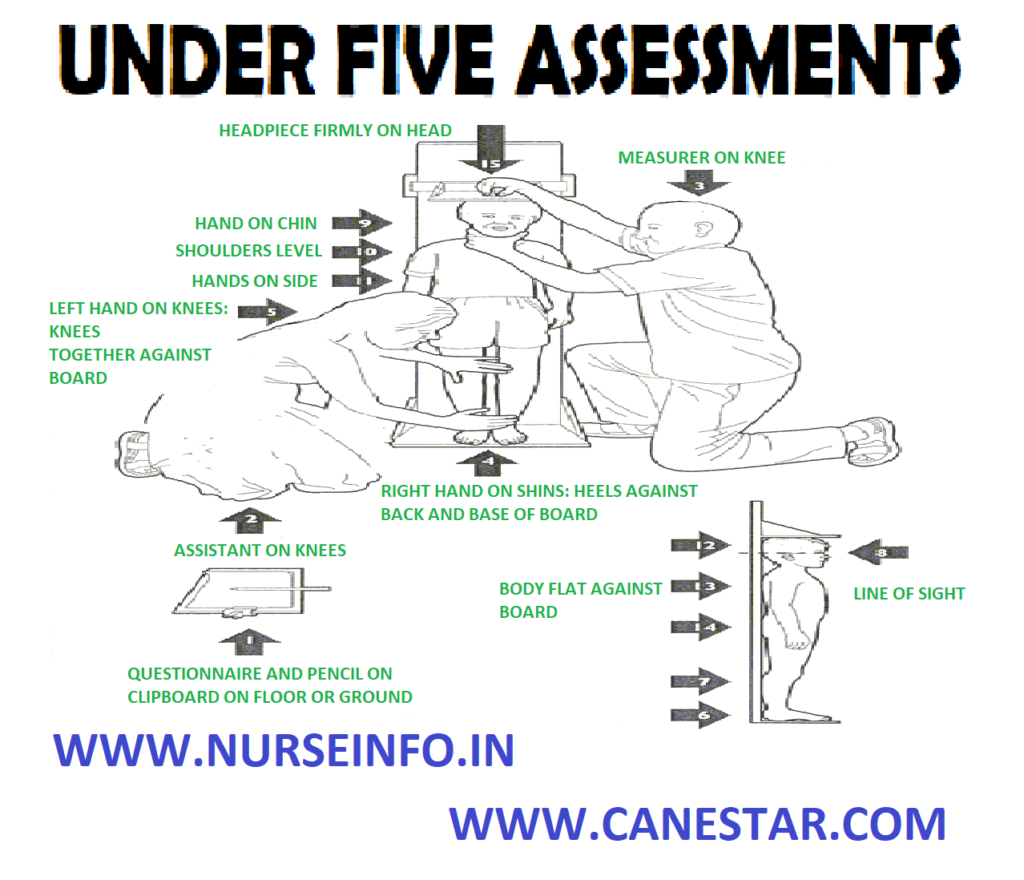
- Weighing and measuring should be provided in a separate area if possible or it may be part of the waiting room
- Isolation area for children with signs and symptoms of illness is essential for every child health clinic

NURSING PROCEDURES LIST CLICK HERE
KEY POINTS
Here are some key points regarding the care of children under the age of five:
- Nutrition: Proper nutrition is crucial for the healthy development of children under five. Breastfeeding is recommended as the best source of nutrition for infants up to six months of age, followed by the introduction of complementary foods while continuing breastfeeding up to two years or beyond. Adequate intake of nutrients such as protein, vitamins, and minerals is essential for growth and development.
- Immunization: Following the recommended immunization schedule is essential to protect children under five from vaccine-preventable diseases. Vaccines help build immunity and prevent the spread of infectious diseases, reducing the risk of illness, disability, and death.
- Hygiene and Sanitation: Good hygiene practices, including handwashing with soap and water, safe food handling, and sanitation measures, are critical for preventing the spread of infections and diseases among young children. Access to clean water and sanitation facilities is essential for maintaining health and preventing waterborne illnesses.
- Healthcare: Regular health check-ups and access to healthcare services are vital for monitoring the growth and development of children under five, detecting and managing health issues early, and providing appropriate treatment and preventive care. Maternal and child health services, including antenatal care, postnatal care, and well-child visits, play a crucial role in promoting child health and well-being.
- Safety and Childproofing: Creating a safe environment for young children is essential to prevent accidents and injuries. Childproofing the home, including installing safety gates, securing furniture and electrical outlets, and keeping hazardous substances out of reach, helps minimize the risk of accidents and promote child safety.
- Stimulation and Play: Providing opportunities for play, exploration, and stimulation is vital for the cognitive, emotional, and social development of children under five. Engaging in age-appropriate activities and spending quality time with children supports their learning and overall well-being.
- Parental and Caregiver Support: Supporting parents and caregivers in providing responsive and nurturing care is crucial for the healthy development of children under five. Providing information, education, and support on child-rearing practices, positive discipline, and early childhood development can empower parents and caregivers to create a nurturing environment for their children.