MENIERE’S DISEASE – Etiology, Signs and Symptoms, Diagnostic Evaluation and Management
Meniere’s disease is a disorder of the inner ear that causes spontaneous episodes of vertigo, a sensation of a spinning motion, along with fluctuating hearing loss, ringing in the ear (tinnitus), and sometimes a feeling of fullness or pressure in ear.
ETIOLOGY
The cause of Meniere’s disease is not well understood. It appears to be the result of the abnormal volume or composition of fluid in the inner ear.
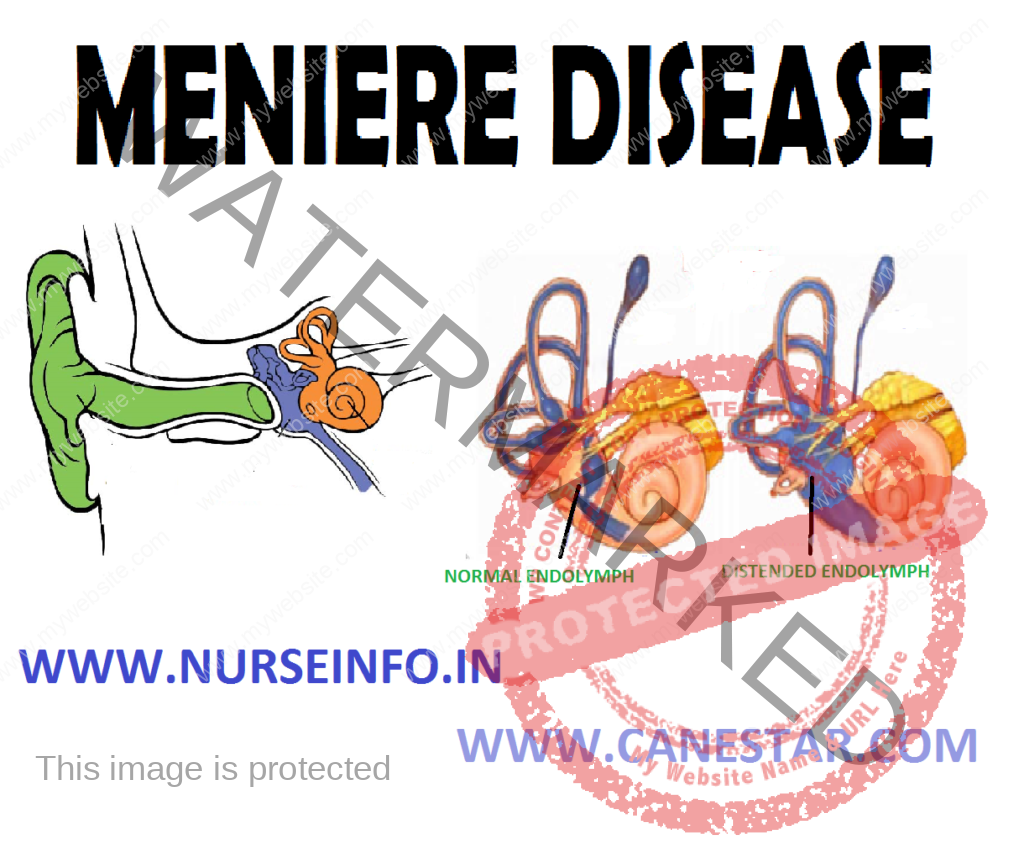
The inner ear is a cluster of connected passages and cavities called a labyrinth. The outside of the inner ear is made of bone (bony labyrinth). Inside is a soft structure of membrane (membranous labyrinth) that is slightly smaller, similarly shaped version of the bony labyrinth. The membranous labyrinth contains a fluid (endolymph) and is lined with hair-like sensors that respond to movement of the fluid.
Meniere’s disease may occur because of the following reasons.
- Improper fluid drainage, perhaps because of a blockage or anatomic abnormality
- Abnormal immune response
- Allergies
- Viral infection
- Genetic predisposition
- Head trauma
- Migraines
SIGNS AND SYMPTOMS
The primary signs and symptoms of Meniere’s disease are:
- Recurring episodes of vertigo: vertigo is similar to the sensation experience if you spin around quickly several times and suddenly stop. Patient feels as if the room is still spinning, and he loses his balance. Episodes of vertigo occur without warning and usually last 20 minutes to two hours or more, up to 24 hours. Severe vertigo can cause nausea and vomiting
- Hearing loss: hearing loss in Meniere’s disease may fluctuate, particularly early in the course of the disease. Eventually, most people experience some degree of permanent hearing loss.
- Ringing in the air (tinnitus): tinnitus is the perception of a ringing, buzzing, roaring, whistling or hissing sound in the ear
- Feeling of fullness in the ear: people with Meniere’s disease often feel aural fullness or increased pressure in the ear
DIAGNOSTIC EVALUATION
A diagnosis of Meniere’s disease requires:
- Two spontaneous episodes of vertigo, each lasting 20 minutes or longer
- Hearing loss verified by a hearing test on at least one occasion
- Tinnitus or aural fullness
- Exclusion of other known causes of these sensory problems
- Physical examination and medical history
Physical examination may include:
- The severity, duration and frequency of the sensory problems
- History of infectious diseases or allergies
- Medication use
- Past ear problems
- General health
- History of inner ear problems in the family
- Hearing assessment
A hearing test (audiometry) assesses how well you detect sounds at different pitches and volumes and how well you distinguish between similar-sounding words. The test not only reveals the quality of hearing but also may help determine if the source of hearing problems is in the inner ear or the nerve that connects the inner ear to the brain.
- Balance assessment
Between episodes of vertigo, the sense of balance returns to normal for most people with Meniere’s disease. But there may be some degree of ongoing balance problems.
There are several tests that assess functioning of the inner ear. Some or all of these tests can yield abnormal results in a person with Meniere’s disease
- Videonystagmography (VNG): this test evaluates balanced function by assessing eye movement. Balance-related sensors in the inner ear are linked to muscles that control movement of the eye in all directions. This connection is what enables us to move head around while keeping our eyes focused on a single point
- In a VNG evaluation, warm and cool water or air are introduced into the ear canal. Measurements of involuntary eye movements in response to this stimulation are performed using a special pair of video goggles. Abnormalities of this test may indicate an inner ear problem.
- Rotary-chair testing: like a VNG, this measures inner ear function based on eye movement. In this case, stimulus to inner ear is provided by movement of a special rotating chair precisely controlled by a computer
- Vestibular evoked myogenic potentials (VEMP) testing: VEMP testing measures the function of sensors in the vestibule of the inner ear that help to detect acceleration movement. These sensors also have a slight sensitivity to sound. When these sensors react to sound, tiny measureable variations in neck or eye muscle contractions occur. These contractions serve as an indirect measure of inner ear function
- Posturography: this computerized test reveals the concerned part of the balance system, vision, inner ear function, or sensations from the skin, muscles, tendons and joints. While wearing a safety harness, you stand barefooted on a platform and keep your balance under various conditions.
- Magnetic resonance imaging (MRI): this technique uses a magnetic field and radio waves to create images of soft tissues in the body. It can be used to produce either a thin cross-sectional ‘slice’ or a 3-D image of brain
- Computerized tomography (CT): this X-ray technique produces cross-sectional images of internal structures in the body.
- Auditory brainstem response audiometry: this is a computerized test of the hearing nerves and hearing centers of the brain. It can help detect the presence of a tumor disrupting the function of auditory nerves.
MANAGEMENT
No cure exists for Meniere’s disease, but a number of strategies may help to manage some symptoms.
Medication for vertigo
- Motion sickness medications, such as meclizine or diazepam, may reduce the spinning sensation of vertigo and help control nausea and vomiting
- Anti-nausea medications, such as promethazine, may control nausea and vomiting during an episode of vertigo
- Diuretic, such as the drug combination triamterene and hydrochlorothiazide. It reduces the amount of fluid the body retains and helps to regulate the fluid volume and pressure in inner ear.
Noninvasive therapies and procedures
Some people with Meniere’s disease may benefit from other noninvasive therapies and procedures, such as:
- Rehabilitation: problems with balance between episodes of vertigo may be reduced by vestibular rehabilitation therapy. The goal of this therapy, which may include exercises and activities that perform during therapy sessions and at home, is to help your body and brain regain the ability to process balanced information correctly
- Hearing aid: a hearing aid in the ear affected by Meniere’s may improve hearing
- Meniett device: for vertigo that is hard to treat, this therapy involves the application of positive pressure to the middle ear to improve fluid exchange. A device called Meniett pulse generator applies pulses of pressure to the ear canal through a ventilation tube. The treatment is performed at home, usually three times a day for five minutes at a time. Meniett device shows improvement in symptoms of vertigo, tinnitus and aural pressure
Middle Ear Injections
Medications injected into the middle ear, and then absorbed into the inner ear, may improve vertigo symptoms. For example, Gentamicin, steroids, such as dexamethasone, also may help control vertigo attacks in some people
Surgical Management
If vertigo attacks associated with Meniere’s disease are severe and debilitating and other treatments do not help, surgery may be an option. Procedures may include:
- Endolymphatic sac procedures: the endolymphatic sac plays a role in regulating inner ear fluid levels. These surgical procedures may alleviate vertigo by decreasing fluid production or increasing fluid absorption. In endolymphatic sac decompression, a small portion of bone is removed from over the endolymphatic sac. In some cases, this procedure is coupled with the placement of a shunt, a tube that drains excess fluid from inner ear
- Vestibular nerve section: this procedure involves cutting the nerve that connects balance and movement sensors in inner ear to the brain (vestibular nerve). This procedure usually corrects problems with vertigo while attempting to preserve hearing in the affected ear.
- Labyrinthectomy: with this procedure, the surgeon removes the balance portion of the inner ear, thereby removing both balance and hearing functions from the affected ear. This procedure is performed only if one already has near-total or total hearing loss
NURSING MANAGEMENT
Nursing Diagnosis
- Risk for injury related to altered mobility because of gait disturbed and vertigo
- Impaired adjustment related to disability requiring change in lifestyle because of unpredictability of vertigo
- Risk for fluid volume imbalance and deficit related to increased fluid output, altered intake and medications
- Anxiety related to threat of, or charge in, health status and disabling effects of vertigo
- Ineffective coping related to personal vulnerability and unmet expectations stemming from vertigo
- Self-care deficits related to labyrinth dysfunction and episodes of vertigo
Nursing Interventions
- Provide nursing care during acute attack
- Provide a safe, quiet, dimly lit environment and enforce bed rest
- Provide emotional support and reassurance to alleviate anxiety
- Administer prescribed medications, which may include antihistamines, antiemetic, and possibly, mild diuretics. Instruct the client on self-care instructions to control the number of acute attacks.
- Discuss the nature of the disorder
- Discuss the need for a low-salt diet
- Explain the importance of avoiding stimulants and vasoconstrictions (e.g. caffeine, decongestants, alcohol)
- Discuss medications that may be prescribed to prevent attacks or self-administration of appropriate medications during an attack, which may include anticholinergics, vasodilation, antihistamines, and possibly, diuretics or nicotinic acid
- A labyrinthectomy is the most radical procedure and involves resection of the vestibular nerve or total removal of the labyrinth performed by the transcanal route, which results in deafness in that ear
- An endolymphatic decompression consists of draining the endolymphatic sac and inserting a shunt to enhance the fluid drainage