MECHANICAL VENTILATION – Definition, Purpose, Indications for Ventilatory Support, Equipment, Positive Pressure Ventilation, Types of Positive Pressure Ventilators, Pressure Cycled, Modes of Mechanical Ventilation, Uses of IMV, Synchronized Intermittent Mandatory Ventilation (SIMV), Special Positive Pressure Ventilation Technique, Newer Modes of Mechanical Ventilation, Pressure Support Ventilation, High Frequency Ventilation and Procedure
Mechanical ventilation has been used for decades to support the respiratory function of patients with various degrees of respiratory distress of failure. Patients who have weak or absent spontaneous respirations usually require mechanical support to assist in ventilation and oxygenation. Because the ventilator is integral life support equipment in the critical care, it is important for the practitioner to know the basic concepts and applications of mechanical ventilation.
HISTORY OF VENTILATOR
The history of artificial ventilation dates back to biblical times where Elisha restored the life of a young boy by supporting respiratory function artificially. Paracelsus in sixteenth century placed a tube in the mouth of a patient and used a fire place bellows to inflate lungs. Successful techniques for artificial ventilation were first developed in 1920s for the administration of anesthetic gases. Endotracheal intubation made the use of ventilator easier. Negative pressure ventilator gained popularity for the use of polio victims. Use of positive pressure ventilation during Scandinavian polio epidemic of 1950s showed that survival rate was better. From 1955 era of modern pressure ventilator started. Mechanical ventilators have come a long way since the days of iron lung machine. Most modern ventilators are capable of carrying out all functions and they are the result of a modification of basic techniques and modalities rather than new ideas.
DEFINITION
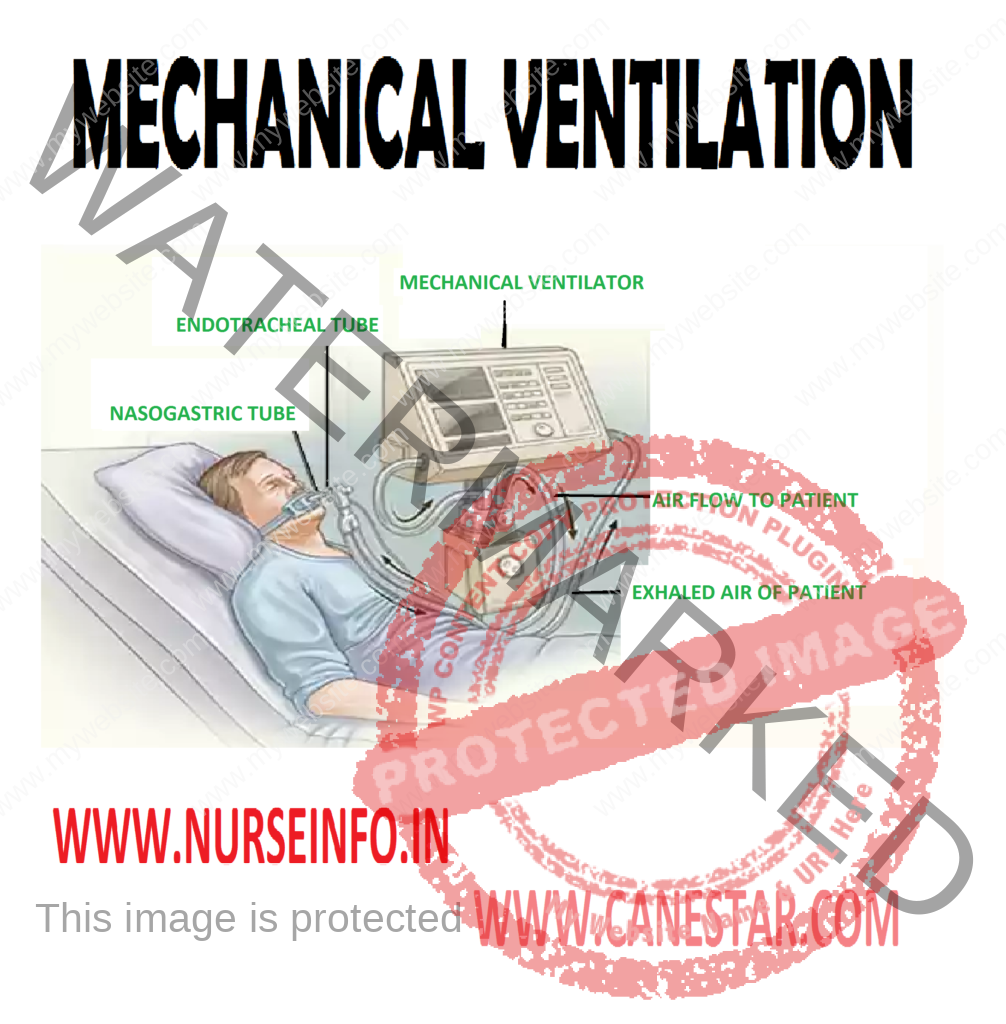
Mechanical ventilation is a device that inflates the lungs by positive pressure which is able to carry out alveolar ventilation and maintain lung mechanics.
PURPOSE
- To establish and maintain effective ventilation
- To prevent complications associated with artificial ventilation
- To ensure position and patency of endotracheal and tracheostomy tube
- To clear and remove secretions from airway
INDICATIONS FOR VENTILATORY SUPPORT
- In upper airway obstruction like if the patient has a paralyzing disease or unconsciousness owing to severe head injury
- In lower airway obstruction respiratory impairment is the result of blockage caused by blood or pus. Other reasons are bronchospasm and edema
- Neuromuscular ventilatory muscle inadequacy occurs when muscles of ventilation are diseased as in myasthenia gravis, poliomyelitis, Guillain-Barre syndrome, snake bite and inadequate reversal of anesthesia. Nerve supply to the intercostals muscles can be interrupted by spinal injury
- Lung disease which prevents proper exchange of oxygen and carbon dioxide as in chest injuries pneumothorax. Infections of lungs, infiltrative lung disease, chronic obstructive lung disease and adult respiratory distress syndrome
- High-risks patients who are potential for developing respiratory failure are given ventilatory support which would help in lessening the work of breathing as in post-operative cardiac surgery, any other major surgery, shock and trauma
- Respiratory arrest respiratory depression to the point of apnea can be produced by changes such as muscle relaxants, opiates, barbiturates, tranquilizers and anti-depressant drugs
Overdose of these drugs and any other systemic condition resulting in respiratory arrest, ventilatory support is indicated.
EQUIPMENT
Bed, locker with necessary articles, ventilator, suction apparatus, continuous monitoring apparatus, resuscitation crash cart with defibrillator
Oxygen giving set and manual ventilation bag (Ambu bag)
Clinical parameters indicating ventilatory support are:
- Respiratory rate >40/minute
- Tidal volume <5 ml/kg
- Vital capacity <15 ml/kg
- PaCO2 <50 mm of Hg with FiO2 >0.60
- PaCO2 >55 mm of Hg with PH <7.25
POSITIVE PRESSURE VENTILATION
Unlike the earlier models of negative pressure ventilators such as druncar and Shaw tank type ventilator (iron lung) recent ventilators function on positive pressure ventilation. Positive pressure is applied at the patient’s airway through an endotracheal or tracheostomy tubes. Clinical use of positive pressure includes intermittent positive pressure ventilation.
Positive pressure brings about, complex change in the body. It may reduce the cardiac output and hypoperfusion of the kidneys with an alternation in urine output. A reduction in venous drainage secondary to increased intrathoracic positive pressure could stimulate OSMO receptors in the hypothalamus to mediate secretion of ADH which in turn will reduce the urine output
TYPES OF POSITIVE PRESSURE VENTILATORS
- Commonly the ventilators are classified by their method of cycling from the inspiratory phase to the expiratory phase in the change over from inspiratory to expiratory phase
- The term cycle is used to indicate a terminating event
Volume cycled: this is the most common form of ventilator cycling. They terminate the inspiratory phase when a designed volume of the gas is delivered into the ventilator circuit (12-15 ml/kg body weight). They deliver the predetermined volume regardless of changing lung compliance. Airway pressure will increase as compliance decreases and it varies from patient to patient and breath to breath. As a safety device many ventilators have a pressure limiting value, fixed or adjustable which prevents excessive build up within the patient ventilator system on any given breath. Depending upon the type of pressure regulating device in use the breath may be terminated before the entire volume has been delivered to the patient. This, however, can be monitored with exhaled volume measuring devices available on most volume ventilators. These devices monitor for leaks in the patient circuit. The common volume cycled ventilators used are Bennet MA 1,2, Boums, LS 104-105, Bournas Bear 1, Ohio 560. Modern ventilators which are compact and computerized are available inn market now.
PRESSURE CYCLED
Terminates the inspiratory phase when preselected airway pressure is reduced. The tidal volume depends upon the patient’s airway resistance and lung compliance and on the peak pressure that has been selected. Use of volume-based alarms are recommended because any obstruction between the machine and lungs that allows a buildup of pressure in the ventilator circuit will cause the ventilator to cycle but the patient will not receive any volume, e.g. Bird mark 6,7,89, 14, 7, Barret PR1 and PR2
As opposed to the old pressure limits ventilator the new machine maintain a predetermined inspiratory pressure during the whole time of inspiration. The delivered tidal volume is dependent on the compliance of the patient’s respiratory system, achieved inspiratory flow and the allowed time for inspiration
Time cycled: the delivered breath is terminated when a preset time has been reached after a pressure limit also is reached and the remainder of the inspiratory phase is in the form of inspiratory pause. These ventilators allow pressure control of inspired fraction of O2 and adequate humidification systems, e.g. Siemens Serio Engstrom
MODES OF MECHANICAL VENTILATION
- Control mode ventilation: the ventilator initiates and controls both the volume delivered and the frequency of breaths. In between, the machine breaths the patient is unable to breathe spontaneously or trigger a ventilator breath. This may result in increase in work of breathing for patients attempting to breathe spontaneously. It is indicated in patients with apnea, drug over dose, spinal cord injuries, central nervous system dysfunction, flail chest, paralysis from drugs and neuromuscular disease. In practice, control combined with other modes is widely used.
- Assist mode: it is a mode of ventilation in which the patient is able to initiate inspiration and to control the frequency of breathing. No minimum level of minute ventilation is provided. The major disadvantage of assist mode was the backup rate if the patient becomes apneic. Once inspiration is initiated ventilation will deliver gas flow until desired volume, pressure or time lime is reached
- Assist/control: it is a combination of assist and control modes. The tidal volume and the rate are preset when the patient’s makes an inspiratory effort the ventilator senses the effort and delivers the preset tidal volume. If the patient fail to initiate inspiration, the ventilator automatically goes into the backup mode and delivers the preset rate and tidal volume until it senses an inspiratory effort. This backup rate ensures minimum minute ventilation in the event of apnea. Assist/control methods are used in neuromuscular disease such as myasthenia gravis or Guillain-Barre syndrome, post-cardiac or respiratory arrest, pulmonary edema, adult respiratory distress syndrome
pH and PaCO2 may be normal and the patient is able to control his respiratory rate and minute ventilation
cycling the ventilation’s normal ventilatory activity and therefore prevents atrophy of the respiratory muscles
- Intermittent mandatory ventilation (IMV): it allows patient to breath spontaneously with the ventilator providing mandatory breaths at a predetermined rate. Ventilator provides mandatory breaths at a predetermined rate at preset tidal volume. Gas provided for spontaneous breathing usually flows continuously through the ventilator circuit
Advantages
- The iatrogenic effects of mechanical ventilation such as barotrauma and decreased cardiac output are reduced
- Higher levels of pulmonary end expiratory pressure can be used because mean intrapleural pressure is lower
- There is less chance for hyperventilation
- IMV can be used as a means of weaning the patient from mechanical ventilation
- Less need for sedation for paralysis of patient on mechanical ventilation
- More even distribution of ventilation and lung blood flow
Disadvantages
- Asynchronous breaths. Mandatory breaths may be imposed on the patient’s spontaneous inspiration or expiration
- Apnea or hypoventilation
USES OF IMV
- Used as a primary means of mechanical ventilation
- Used in patients who have respiratory patterns that use asynchronous with the control mode
- Used in patients who hyperventilate on the assist/control mode
- Used in patients who require some respiratory support but are able to breathe spontaneously
- Used as a means of weaning patients from mechanical ventilation
SYNCHRONIZED INTERMITTENT MANDATORY VENTILATION (SIMV)
Allow patient to breath spontaneously through the ventilator circuit. At a preselected time, a mandatory breath is delivered. The patient may initiate the mandatory breath with his own inspiratory effort and the ventilator breath will be synchronized with the patients effort will be assisted. If the patient does not provide inspiratory effort the breath will be delivered as controlled. Gases provided for spontaneous breathing is delivered through a demand regulate which is activated by patient
It is comfortable for the patient. Disadvantages and clinical uses are same as chart of IMV. In addition, it is used whenever lack of synchronous breathing seems to affect patient’s ability to be weaned
SPECIAL POSITIVE PRESSURE VENTILATION TECHNIQUE
- Posture end expiratory pressure (PEEP): It is a mode of therapy used with mechanical ventilation where pressure during mechanical ventilation is maintained above atmosphere at the end of exhalation resulting in an increased functional residual capacity. Airway pressure is positive throughout the ventilator cycle. When use to treat patients with diffuse lung disease PEEP improves compliance, decreases dead space
Uses: used to increase the surface area to prevent collapse of alveoli and development of atelectasis. Used to decrease intrapulmonary shunt
Advantages
- Lower level of FiO2 concentration of inspired oxygen is necessary with PEEP
- It is helpful in reducing the transudation of fluid from the pulmonary capillaries in situations where pressure is increased as in left heart failure or when the alveolar capillary membrane is damaged as in adult respiratory distress syndrome
- Increased lung compliance resulting in decreased work of breathing
Disadvantages
- Due to the increased airway resulting in over distension of alveoli can result in decreased cardiac output due to decreased venous return
- The increased airway pressure can result in rupture of the alveoli which may cause pneumothorax or subcutaneous emphysema
- The decreased venous return stimulates the production of antidiuretic hormone thereby the urine output is reduced
Monitoring of the patient on PEEP should include signs and symptoms of pneumothorax such as increased pulmonary artery pressure, decreased lung movement, diminished breath sounds, and signs and symptoms of decreased venous return which includes decreased arterial pressure, decreased cardiac output and decreased urine output.
- Continuous positive airway pressure (CPAP): it has the same physiological characteristics of PEEP. It provides positive airway pressure during all parts of respiratory cycle but refers to spontaneous ventilation rather than mechanical ventilation. CPAP is delivered through ventilator circuit or through a separate CPAP circuit which does not require ventilator. It is indicated for patients who are capable of marinating adequate tidal volume but are not able to maintain tissue oxygenation
NEWER MODES OF MECHANICAL VENTILATION
- Pressure control ventilation: a pressure limited time cycled ventilator is used. (Servo 900c or Puritan Bennet 7200a) The Servo controlled valves were the key to the development of the pressure control time cycled mode now available. Specific inspiratory pressure and inspiratory time is set. The ventilator delivers a flow of gas until the pressure is reached which is maintained within the lung for the set inspiratory time. As in assist control mode, the patient is able to initiate a breath and in the event of apnea a backup rate will support the patient’s respirations. But, with changes in airway resistance and lung compliance the delivered tidal volume varies. With pressure control ventilation the initial flow is high due to the maximum pressure difference between the inspiratory pressure delivered by the ventilator and the pressure present inside the lung at the beginning of the inspiratory cycle. With the subsequent increase in intrathoracic pressure, the pressure difference diminishes so also the inspiratory flow. The flow pattern is called decelerating inspiratory flow as against the constant flow pattern in traditional ventilation. The absolute rate of inspiratory flow is influenced by the resistance of the airways. If the resistance of high, the flow is reduced, if it is low, the flow is increased. Deceleratory flow leads to an early and sustained ultra-alveolar pressure whereas in the traditional ventilation with constant inspiratory flow intra-alveolar pressure is increased; thereby the pulmonary gas exchange in diseased lung is better with this mode.
The rapid introduction of gas into the airway may be uncomfortable for patient and may require sedation/paralysis.
Pressure control ventilation is indicated in all clinical situations requiring mechanical ventilation as this mode provides most efficient gas exchange at the lowest inspiratory pressure
- Inverse ratio ventilation: it is an alternative method of providing ventilatory support to a group of patients with refractory hypoxia. As against the conventional methods, the duration of inspiratory phase is revered. Inspiratory-expiratory ratio becomes 4:1 which result in a shortened expiratory time. The incomplete exhalation causes a PEEP like effect which in turn causes, the alveolar pressure to remain positive throughout the entire respiratory cycle. This constant pressure prevents the alveoli from collapsing at the end of exhalation
Indications
- Diffuse lung injury
- Refractory hypoxemia
- Hemodynamic stability
Contraindications
- A nondiffuse lung disease such as lobar pneumonia
- Obstructive pulmonary disease
- Presence of copious secretions
A pressure limit time cycled ventilator in the pressure control mode is used when implementing TRV
Following parameters are monitored when patient is on TRV
PRESSURE SUPPORT VENTILATION
- Heart rate, blood pressure, cardiac output
- Hemodynamic measurements including those obtained from pulmonary artery catheter
- Pulse oximeter and capnography
- Arterial blood gases
- Airway pressure
- All ventilator parameters
The patient must meet the criteria for IRV and the staff should have proper understanding of the technique, equipment and operation
Pressure support ventilation is a mode of ventilation that provides augmentation of spontaneous breaths with selected levels of positive pressure. As the patient initiates a breath the preselected pressure is reached quickly. Unlike other modes, PSV requires the patient to take a continuous effort in order for the ventilator to deliver pressure support. It is similar to intermittent positive pressure breathing
Indications
- Patients who have difficulty in weaning using conventional method
- Anxious patients
- Patients who have less than optimal artificial airway
- Patients with chronic obstructive pulmonary disease
- Weak patients
HIGH FREQUENCY VENTILATION
High frequency ventilation refers to any form of mechanical ventilation that functions at a frequency of at least four times the normal respiratory rate. It provides small tidal volumes and less peak inspiratory pressure. To compensate for this, rate is increased
High Frequency Positive Pressure Ventilation
It is positive pressure ventilation delivered at a rate of 60-100 breaths per minute with tidal volume of 3-5 ml/kg through a system that does not involve gas entrapment
Indications
- Patients with pulmonary air link
- Pneumomediastinum
- Respiratory failure or ARDS
- High frequency Jet ventilation consists of intermittent delivery of high pressure gas about 140-2800 cm of 420 through a small bore injector cannula placed in the proximal end of endotracheal tube
- Suction tubing and catheter to be transparent so that nature of aspirate can be observed
- Ensure that vacuum pressure Is not more than 120 mm Hg in adult and 100 mm Hg in children
- Endotracheal tube to be rotated daily, to prevent pressure ulcer on patient’s lip or tongue
- Inflation of endotracheal/tracheotomy tube to be monitored regularly
- Positioning of endotracheal/tracheotomy tube to be monitored regularly
- Symptoms to be reported immediately
- Aseptic technique to be used when carrying out procedures involving tracheotomy or endotracheal tube
- Functioning of ventilator alarms to be checked at beginning of each shift
- Ventilator settings to be checked and recorded every hour
- Tubing’s leadings from ventilator to patient must be checked at least every hour and accumulated moisture to be removed
- Humidifier to be kept adequately filled with sterile distilled water
- Tuning and water in humidifier must be kept scrupulously clean, including connections and adapters, which are to be removed for sterilization every 24 hours
- In presence of possible ventilator fault, nurse must always first check clinical state of patient. If this is satisfactory then proceed to detect fault
- If patient shows signs of insufficient ventilation, nurse must start manual ventilation whilst waiting for assistance
- Avoid positioning ventilation tubes above patient’s head to avoid water entering lungs
- Humidifier to be changed daily and sterile water to be used
- Weaning is usually commenced in day time rather than at night
PROCEDURE
Care of ETT/Tracheostomy
- Secure positioning of ETT/tracheostomy tube with tape or adhesive plaster
- Inflate cuff once correct positioning has been confirmed
- Cuff is inflated with air using a syringe until a “hiss” is heard on auscultation (minimum air leak technique)
Maintaining Ventilation
- Effects of ventilation are assessed by observing patient’s color, chest movement, blood pressure, pulse rate/oxygen saturation and ventilatory measurements such as expired minute and tidal volume, airway pressure and rate of ventilation
- Ventilators make characteristics sounds during inspiration and expiration which nurse must be capable of identifying
- Ensure patient has adequate fluid and calorie intake
- Administer sedation as prescribed to ensure adequate artificial ventilation and promotion of rest
Signs of Adequate Ventilation
- Improvement in skin color and oxygen saturation more than 90%
- Rhythmic expansion of chest with expiratory phase longer than inspiratory phase
- Normal pulse, change in pulse rate may indicate decreased cardiac output due to increase in intra-thoracic pressure
- Steady blood pressure. A drop in blood pressure may reflect decreased cardiac output
- Audible respiratory rhythm
- Absence of any abnormal neurological signs
- Absence of hyperventilation or hypoventilation
Signs of Inadequate Ventilation
- Breathing occurs out of sequence with ventilation and patient is restless, perhaps diaphoretic, flushed or cyanosed
- First signs of ventilatory inadequacy and hypoxia may be tachycardia and hypertension
- If change in recordings of ventilatory volume occurs check airway pressure and rate of ventilation
- If increase in minute volume, check for leaks in cuff seal, connections and tubing
- If decrease in airway pressure occur check for leak in circuit
- If increase in peak airway pressure occur check for obstruction such as secretions, kinking, pooling of water, patient bitting tube slipped into a main stem of bronchus, pneumothorax
Suctioning
- Explain procedure to patient/family
- Frequency of suction to be carried out depending on patient’s pulmonary state
- Tracheal suction is an aseptic procedure. Sterile catheter and one sterile glove to be used for each suctioning episode/session
- Suction is applied while catheter is being withdrawn using intermittent technique, not more than 10 to 15 seconds
- When secretions are tenacious, instill 1 to 3 ml. sterile normal saline 0.9 percent into endotracheal/tracheostomy tube to liquefy and make removal easier
Weaning
- Inform patient that this is a progressive step in treatment
- Repeatedly encourage and reassure patient to avoid fear or exhaustion
- Withhold sedation and muscle relaxant as ordered by doctor
- Watch for respiratory distress, hypoxia, tachycardia, tachypnea, cyanosis, and hypotension and drop in oxygen saturation
Routine Nursing Care
- Give daily bed bath and change bed linen, if soiled
- Provide 2 hourly attentions to pressure sites by turning and repositioning of patient
- Four hourly oral hygiene and whenever needed
- Four hourly eyes care. Instill artificial tears and cover with Jaconet gauze/plastic foil, to prevent corneal abrasions
- Check and record vital signs every hour
- Measure blood, intravenous transfusion and fluid intake every hour
- Measure blood loss, urine, nasogastric, aspirate, etc. every hour
- Change drainage bags, chest drainage bottles and tubing’s as required
- Maintain intake/output chart every shift
- Eight hourly aseptic urinary catheter toilet
- Assess bowel action every third-day
- Eight hourly wound dressings
- Change the tape anchoring ETT and Ryles tube
- Change intravenous administration sets and dressing of puncture sites every day
- Change suction bottle and connecting tubing everyday
- Change ventilator circuit tubing, connections and adapters everyday
- Record patient’s condition and events that have occurred during each shift in nurse’s progress sheet
- Give detailed hand over to nurse on following shift
Psychological Aspects of Patient’s Care
- Endeavor to allay patient’s and relatives anxiety fears and clear doubts as necessary
- Motivate patient and relatives to participate in daily care activities
- Promote good relationship with patient/family and encourage them to express fears, stress factors/feelings
| ADVANCED CARDIAC LIFE SUPPORT |
| CARDIOVERSION |
| CARDIAC DEFIBRILLATION |
| PACEMAKERS |
| TEMPORARY PACEMAKER THERAPY |
| PERMANENT PACEMAKER IMPLANTATION |
| ARTERIAL BLOOD GAS ANALYSIS |
| VENTILATOR SETTING UP |
| VENTILATOR WEANING |
| PERCUTANEOUS SUPRAPUBIC PUNCTURE |

