BOWEL ELIMINATION – Factors Affecting and Common Problems in Bowel Elimination (Bristol Stool Chart and Color of Stool and its causes)
Defecation is the expulsion of feces from the anus and the rectum. It is also called a bowel movement. The peristaltic waves move the feces into the sigmoid colon and the rectum, the sensory nerves in the rectum are stimulated and the individual becomes aware of the need to defecate.
There are two centers governing the reflex to defecate. One is situated in the medulla and subsidiary one is in the spinal cord. When parasympathetic stimulation occurs, the internal anal sphincter relaxes and the colon contracts. The defection reflex is stimulated chiefly by the fecal mass in the rectum. When the rectum is distended the intrarectal pressure rises, the defecation reflex is stimulated by the muscle stretch, and the desire to eliminate results.
FACTORS AFFECTING BOWEL ELIMINATION
Age and Development: there is a marked difference between the stools of an infant and an older person. The very young are unable to control elimination until the neuromuscular system is developed, usually between the ages of 2 to 3 years.
Daily Patterns: most people have regular patterns of bowel elimination which include frequency, timing considerations, position and place changes in any of these may upset a person routine and actually lead to constipation
Lifestyles: many individual’s family and sociocultural variables influences a person’s usual elimination habits. The long-term effect of bowel training, the availability of toilet facilities, embarrassment about odors and need to privacy, also affect the fecal elimination patterns.
Fluids: both the type and amount of fluid digested affect elimination. Healthy fecal elimination is facilitated by a daily intake of 2000 to 3000 ml.
Activity and muscle tone: regular exercise improves gastrointestinal motility and muscle tone while inactivity decreases both. Adequate tone in the abdominal muscles, the diaphragm and the perineal muscles is essential to case in defecation.
Psychological factors: emotional stress affects the body in many ways. Persons with anxiety causes increased intestinal motility and persons with depression causes slower intestinal motility resulting in constipation
Pathological conditions: spinal cord and head injuries decrease sensory stimulation for defecation. Impaired mobility limits the patient’s ability to respond to the urge to defecate. Ribbon like stools in appearance due to tumor in the colon
Medications: narcotic analgesics cause constipation by decreased gastrointestinal mobility. Many medications have diarrhea as undesirable side effect
Diagnostic procedure: barium salts used in radiologic examinations. It hardens if allowed to remain in the colon, producing constipation and sometimes an impaction
Surgery and anesthesia: direct manipulation of the bowel during abdominal surgery inhibits peristalsis causing a condition termed as paralytic ileus. General anesthetic agents that are inhaled also inhibit peristalsis by blocking the parasympathetic impulses to the intestinal muscle
Irritants: spicy foods, bacterial toxins and poisons can irritate the intestinal tract and produce diarrhea and often large amounts of flatus
Pain: patients who are experience discomfort when defecating. E.g. following hemorrhoid surgery will often suppress the urge to defecate to avoid the pain
COMMON PROBLEMS IN BOWEL ELIMINATION
Constipation: it refers to the passage of small, dry hard stool or the passage of no stool for a period of time. The causes are irregular defecation habits, inappropriate diet, insufficient fluid, insufficient exercises and increased psychological stress
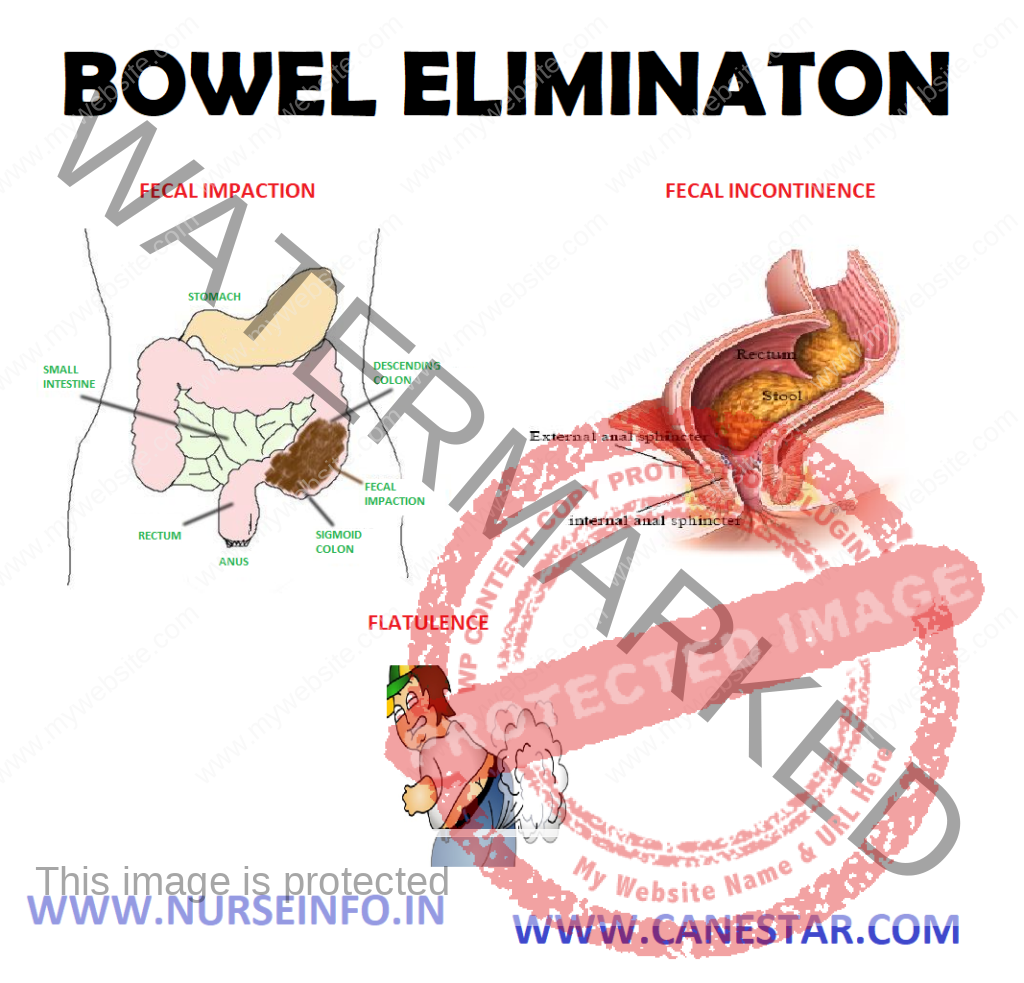
Fecal impaction: it is a mass or collection of hardened feces in the folds of the rectum. The causes are prolonged retentions and accumulation of fecal material, poor defecation habits and constipation and medication
Diarrhea: it refers to the passage of liquid feces and an increased frequency of defecation or it is the discharge of frequent loose stool to the rapid passage of content through the intestines. The causes are emotional stress and infection
Fecal incontinence: it refers to loss of voluntary ability to control fecal and gaseous discharge through the anal sphincter or inability to control the expulsion of feces. The causes are spinal cord trauma and tumors of the external sphincter muscles
Flatulence: it is the presence of excess in the intestine and leads to stretching and inflation of the intestine (intestinal distension) air or gas in the gastrointestinal tract is called flatus
BRISTOL STOOL CHART
Type 1: separate hard lumps, like nuts (hard to pass)
Type 2: sausage-shaped, lumpy
Type 3: sausage shaped, cracks on surface
Type 4: sausage or snake-like, smooth and soft
Type 5: soft blobs with clear-cut edges (easy to pass)
Type 6: fluffy pieces with ragged edges, mushy
Type 7: watery, no solid pieces (entirely liquid)
TYPES OF STOOL COLOR AND ITS CAUSES
GREEN: it is proven that during this condition, food is moving through the large intestine too quickly, such as due to diarrhea. As a result, bile does not have time to break down completely
Dietary Causes: if someone eats more green leafy vegetables, green food coloring such as in Kool-Aid or popsicles, it is in high-risk of developing green stool
PALE OR CLAY-COLORED: there is commonly caused by a lack of bile. In most cases, it is indicating a bile duct obstruction
Dietary Causes: certain medications, such as large doses of kaopectate and other antidiarrhea drugs
YELLOW, GREASY, FOUL-SMELLING: excess fat in the stool, such as due to a malabsorption disorder
Dietary causes: sometimes the protein gluten, such as in celiac disease. But see a doctor for evaluation
BLACK: bleeding in the upper intestinal tract, such as the stomach
Dietary causes: iron supplements, pepto-bismol, black licorice
BRIGHT RED: bleeding in the lower intestinal tract, such as the large intestine or rectum
Dietary causes: red food coloring, beets, tomato juice or soup, red Jell-O
HOT APPLICATION & COLD APPLICATION
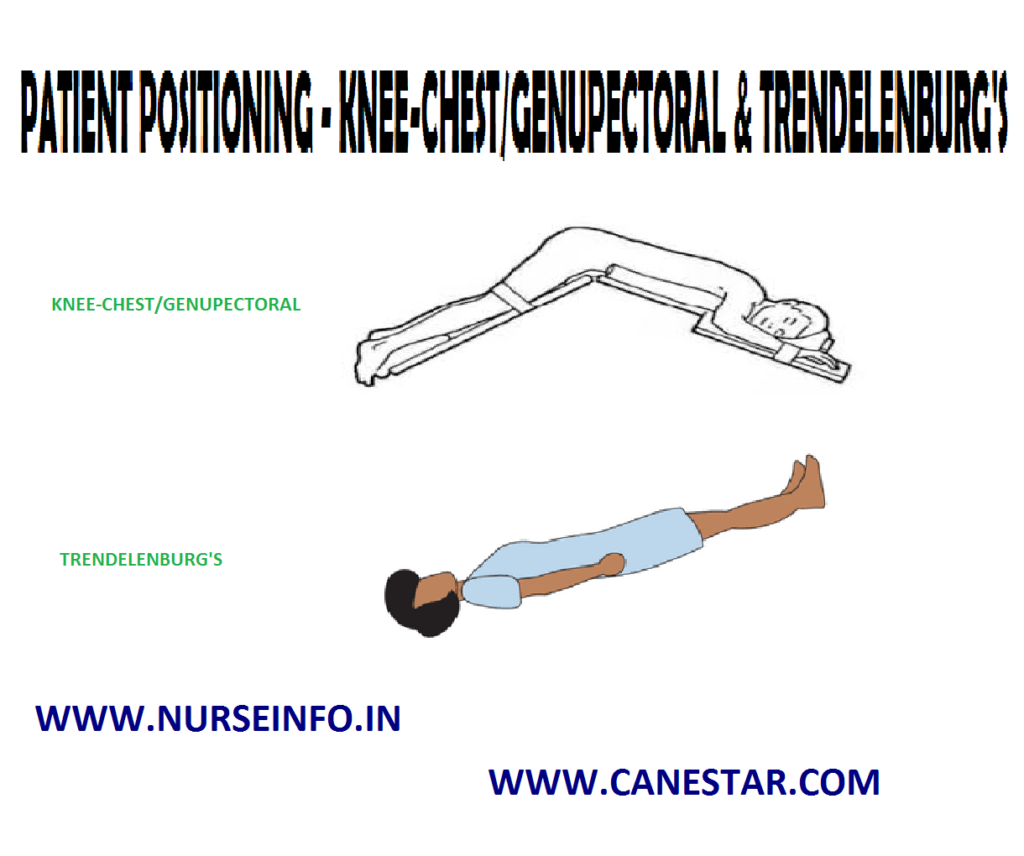
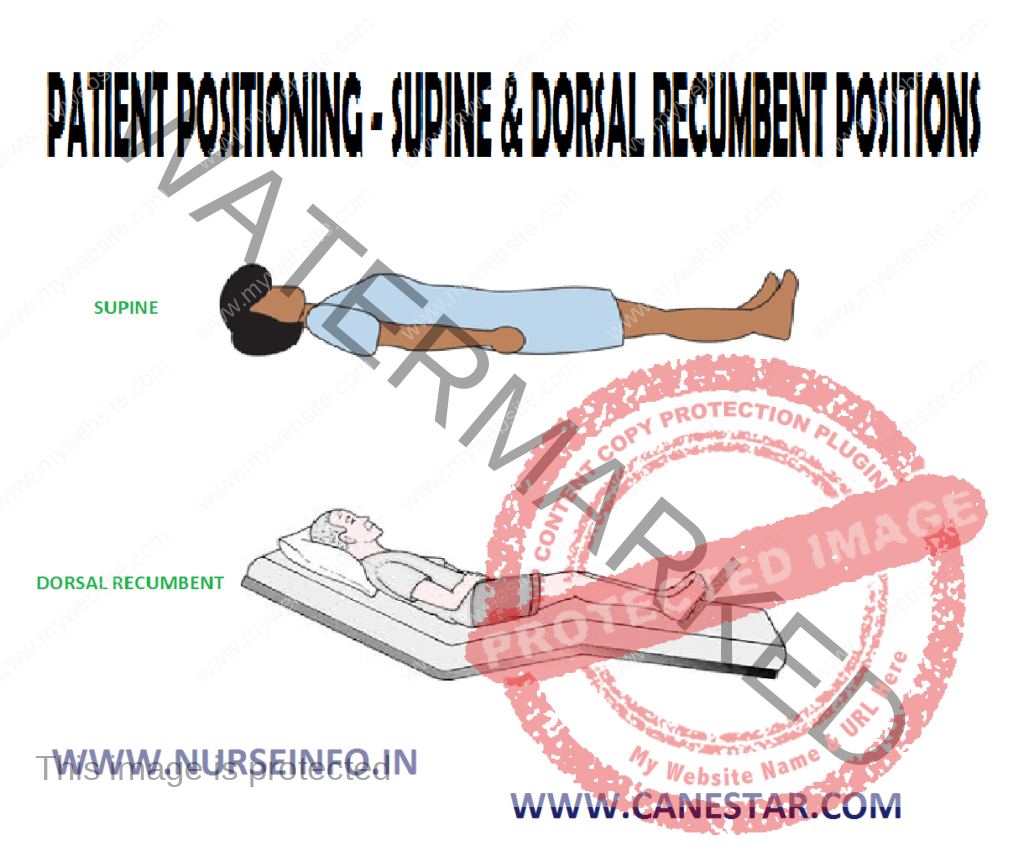
PATIENT POSITIONING , COMFORT DEVICES