AIDS (Acquired Immuno Deficiency Syndrome) – General Characteristics, Route of Transmission, Diagnosis, Clinical Features and Management
General Characteristics
AIDS is the name given to a group of disorders related to immunodeficiency produced as a result of the infection by the Human Immunodeficiecy Virus (HIV). The syndrome was first described in 1981 in LosAngeles in male homosexuals. In a short span of twenty four years, it has spread all across the globe, affecting various spheres of human life. AIDS is the final consequence of various changes that take place in the immune status of the individual and is characterized by the occurrence of opportunistic infections and specific malignancies.
The Causative Organism
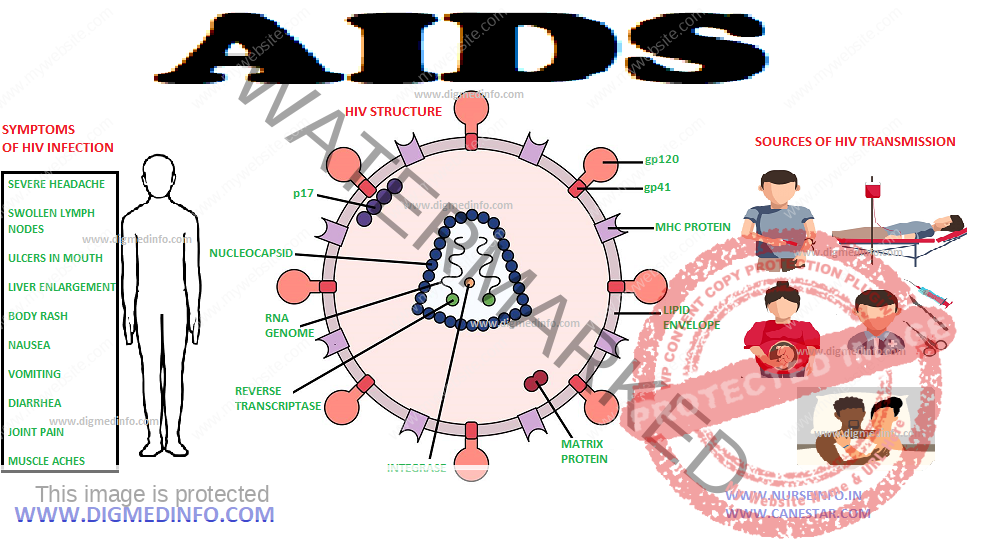
The disease is caused by infection with HIV which is a retrovirus and belongs to the family of lentiviruses. Infections with lentiviruses typically show a chronic course of disease, a long period of clinical latency, persistent viral replication and involvement of the central nervous system. There are many viruses which are classified under this name. HIV-1 and HIV-2 are the major ones. Using electron microscopy, HIV-1 and HIV-2 are almost similar. However, they differ with regard to the molecular weight of their proteins, as well as having differences in their accessory genes. Both HIV-1 and HIV-2 replicate in CD4+ T cells and are regarded as pathogenic, HIV-2 being less pathogenic. HIV-1 is subdivided into groups: M (for main) and O (for outlier), antigenically. Within group M are the vast majority of HIV-1 strains subdivided into subtypes (currently 10: AJ) based on genetic variation. HIV-1 subtype B is more prevalent in homosexuals and IV drug users. However most of the ongoing HIV-1 epidemic around the world is due to non-B subtypes, especially subtype C in sub-Saharan Africa and India. But almost all subtypes have been identified in all parts of the world. HIV viruses are RNA viruses. HIV-1 viral particles have a diameter of 100 nm and are surrounded by a lipoprotein membrane.
During the process of budding, the virus may incorporate, different host proteins, such as HLA class I and II proteins, or adhesion proteins from the membrane of the host cell into its lipoprotein layer.
HIV has greatest affinity towards CD4 receptor bearing T helper lymphocyte group. Two newly identified proteins found on immune cells, CCR5 and fusin (also known as CXCR4) are considered as co-receptors. Certain chemokines are also considered important in modulating the entry of virus into the CD4 cell. After HIV successfully attaches and fuses with the cell, the RNA strands are transcribed to DNA by the timely activation of reverse transcriptase, a viral enzyme. The DNA strands thus formed in the cytoplasm migrate to the nucleus and integrate with the human DNA(with the help of enzyme integrase). This is an irreversible bonding and leads to the beginning of a permanent HIV infection.
The integrated human CD4 cell may take various routes. Some of them are detected by the person’s immune system and are eliminated promptly. Some of them get activated against other antigens or allergens and start producing chemical mediators. When parts of the DNA correspond to that of the virus, the proteins so produced will contain the amino acid sequences needed for the virus replication too. These ‘viral’ proteins are cleaved into correct sequence by the enzyme protease. The newly synthesized viral proteins acquire their coating from the CD4 cell surface and ‘bud out’ damaging the cell membrane. This leads to significant damage to the cells and they are destroyed in large numbers. Some of the cells undergo fusion and form syncitia. Some may be destroyed by cell mediated, complement mediated or antibody dependent cytotoxic mechanisms. Some CD4 cells undergo apoptosis (programmed and premature cell death). Thus the virus infection over a period of years leads to fall in the number of CD4 cells. The virus can also produce direct effects on cells in the brain, heart and bowel and reticulo endothelial system. HIV can replicate aggressively and upto 10 billion virus particles may be produced in a day with an average half life of 6 days.
The CD4 count in a normal person is between 800 and 1200 cells per cmm in peripheral blood. The CD4 cell is responsible for the smooth and coordinated function of all arms of the immune system. Once the CD4 function is compromised, various abnormalities occur. Both physiologic and dysregulated activation contribute to the profound immune activation and accelerated cell death that characterizes HIV infection. In early HIV infection, CD8+ T-cell numbers tend to increase, reflecting expansion of memory CD8+ T cells, particularly HIV reactive cells. CD8 cell expansion persists until far advanced stages of HIV disease, when all T-cell numbers tend to fall. A number of immunological abnormalities have been described including:
1. leukopenia and lymphopenia.
2. Loss of T4 lymphocytes from the peripheral blood.
3. hypergammaglobulinemia.
4. Skin anergy.
5. Decrease in lymphocyte proliferation, cytotoxic T cell response and antibody production to new antigens.
6. elevated levels of immune complexes, interferon and Beta 2 microgobulin
Immunodeficiency manifest in three different patterns:
a. reactivation of dormant infections like tuberculosis and herpes infections
b. infections by opportunistic pathogens
c. atypical manifestations of common infections.
The immune dysregulation also leads to development of specific malignancies such as Kaposi’s sarcoma related to HIV infection
Route of Transmission
HIV is susceptible to destruction by many physical and chemical agents. Close contact and exchange of blood or body fluids is necessary for transmission. The most rampant route is sexual intercourse. Male homosexuals practicing anal sex have the highest risk. Heterosexual anal sex, heterosexual vaginal sex, oral sex and sex using condoms have been stratified in the decreasing order of risk involved. The infection is common amongst IV drug users in whom sharing of contaminated needles, syringes and drugs is the risky factor. The infection can also be transmitted from the mother to the child during pregnancy, at the time of labor or during breast feeding. The transmission is most effective following transfusion of infected blood. Occasionally needles and sharps used in hospitals can act as sources of infection to health care professionals if proper precautions are not taken. HIV does not spread through casual contact, furniture, touching, sharing the food, utensils, toilet or through air or water.
Transmission by sexual intercourse is increased in the presence of other sexually transmitted diseases leading to ulcerative or inflammatory lesions in the genitalia. HIV infected mothers transmit the disease to their babies. Efficiency of transmission depends upon the viral load and clinical stage of the mother, the nature of delivery and time spent in labor. It can vary from 14 to 40%. The risk of transmission by accidental needle pricks in hospitals is around 0.3%.
DIAGNOSIS
HIV infection is a laboratory diagnosis and is made by demonstration of
i. HIV antibodies by ELISA or solid state card/spot tests
ii. Circulating antigens (p24) or
iii. The viral RNA itself by PCR –qualitative and quantitative- in peripheral blood.
Since false positive tests are not uncommon, it is advisable to repeat the tests using different types of ELISAs or different antigens before labelling an asymptomatic person as positive. If clinical symptoms have manifested two positive tests are considered enough.
Fallacies of the tests:
1. The test become positive only after the ‘window’ period i.e. 4-6 weeks or more after infection, by which time only the antibodies appear.
2. In the late stage when antibodies are too low, the tests may be only weakly positive or even negative.
Note: Testing for HIV should be done after counseling the patient and getting his permission.
AIDS is defined as the presence of one of the AIDS defining conditions or a decline of CD4 cells to less than 200 per cmm in an HIV infected person.
CLINICAL FEATURES
The spectrum of diseases caused by HIV is quite wide.
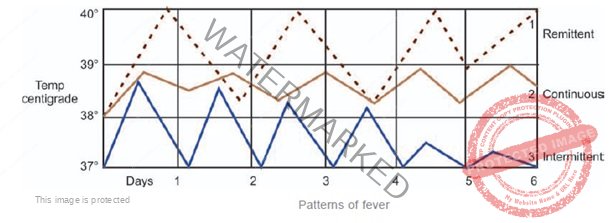
The clinical patterns are grouped into four stages.
• Acute Retroviral syndrome
• Asymptomatic stage
• Early symptomatic stage
• Advanced immunodeficiency
Acute retroviral syndrome (also called Primary HIV infection or seroconversion illness) occurs 2-6 weeks after the entry of HIV into human body. The illness is associated with fever, papular eruptions, arthralgia, lymph node swelling and oral ulcers
The CD4 count falls and viral load increases during this period. The symptomatic phase of acute HIV-1 infection lasts between 7 and 10 days, and rarely longer than 14 days. The severity and duration of symptoms have prognostic implications. Severe and prolonged symptoms are associated with more rapid disease progression, which may be unnoticed in the majority of cases. The infected person recovers completely to an asymptomatic stage with the return of CD4 count to normal but becomes IV antibody positive thereafter.
In the next few years many changes take place in the immune system even though the person is grossly asymptomatic. Immune mediated events like lymph node enlargement, thrombocytopenia, demyelinative disorders of central nervous system, occur with increasing frequency. Most of these are because of misdirected immunologic activity. The occurrence of persistent generalized lymphadenopathy (defined as enlargement of two or more extra inguinal lymph nodes of size 2-3 cm persisting for more than a month) is common at some time in this stage.
As the CD4 count drops to below 500 cells per cmm the person experiences reactivation of dormant organisms like tuberculosis (pulmonary and extra pulmonary), herpes zoster, disseminated herpes, molluscum contagiosum etc. Fungal infections of the genital tract, extensive non genital warts, exaggerated insect bite reactions on the exposed skin etc. are seen in this stage.
As the CD4 count drops below 200 cells per cmm, the opportunistic infections appear. This is also the time when neoplasms like high grade B cell lymphoma, Kaposi’s sarcoma, cervical intra-epithelial neoplasia and primary CNS lymphoma appear. Many infections which remain localized in immunocompetent subjects tend to become disseminated (e.g. M.tuberculosis, Toxoplasma gondii, Cytomegalovirus, Cryptococcus neoformans and Histoplasma capsulatum).
Respiratory System in AIDS
Respiratory system gets involved in almost all patients at some stage. The most important among these are Pneumocystis carinii Pneumonia (now re-named as P. jiroveci) and tuberculosis
Cutaneous Manifestations
Cutaneous manifestations these are quite common in AIDS. A broad spectrum of cutaneous infections caused by viruses, bacteria, fungi, protozoa, and parasites as well as many unusual manifestations of common dermatoses is seen.
Acute primary HIV infection may lead to a transient, generalized, morbilliform eruption on the trunk and the arms. With the person developing immunosuppression, nonspecific skin changes occur. These include common disorders with atypical clinical features, including recurrent varicella zoster, numerous hyperkeratotic warts, treatment-resistant seborrheic dermatitis, and oral hairy leukoplakia.
Chronic Herpes simplex virus (HSV) and Cytomeglovirus (CMV) infections, mycobacterial infections and mucocutaneous candidiasis occur in late stages.
Kaposi’s sarcoma (KS).
This was the first malignancy detected to be associated with HIV infection. The worldwide prevalence of KS in patients with AIDS may approach 34%. Most of the patients are homosexual men. KS is due to proliferation of endothelial cells induced by Human herpes virus type 8. KS begins as pink macules that become disseminated and palpable. Purplish or brown macules and plaques may become nodular. Mucosal involvement is common. The clinical progression of KS in patients infected with HIV is more aggressive than the other clinical types of KS.
Other malignancies can also occur more commonly with HIV infection. AIDS-related B-cell non-Hodgkin’s lymphomas may lead to skin nodules. Anal carcinoma and cervical intraepithelial neoplasia are papillomavirus associated tumours. These tumours tend to be more progressive and aggressive. An increase in squamous cell carcinoma of the anal mucosa has been reported, especially in young homosexual men. Intraoral or multiple squamous cell carcinoma, Bowen disease, and metastatic basal cell carcinoma have occasionally been reported.
Malignant melanoma occuring in patients with HIV is more aggressive than in individuals without HIV. Children with AIDS have a higher risk of developing leiomyosarcoma, although the incidence is still low in this population.
Fungal infections occur extensively on the skin and mucous membranes. Recurrent and persistent mucocutaneous candidiasis is common. Recurrent vaginal candidiasis can occur in any stage of the disease. In adults, generalized dermatophytosis, or tinea capitis, which is typically caused by Trichophyton rubrum is common. Onychomycosis in HIV infected may continue for many years.
Deep fungal infections like cryptococcosis, histoplasmosis and coccidioidomycosis may disseminate to the skin, usually as hemorrhagic papules or nodules.
Other infections: Mycobacterium tuberculosis; Mycobacterium avium-intracellulare complex; and, rarely, Mycobacterium kansasii may present as acneiform papules and indurated crusted plaques. Impetigo and folliculitis may be recurrent and persistent in HIV disease, particularly in children. Disseminated furunculosis, gingivitis, gangrenous stomatitis, and abscess formation can occur. Bacillary angiomatosis, which is caused by Bartonella henselae and rarely by Bartonella quintana, usually manifests as red papules and nodules. Atypical or Norwegian scabies, which is characterized by widespread hyperkeratotic, scaly maculopapular eruptions or crusted plaques, can occur. Seborrheic dermatitis like eruptions are observed in 83% of patients with AIDS. Seborrheic dermatitis may be the initial cutaneous manifestation of HIV disease. The eruption, which is characterized by widespread inflammatory and hyperkeratotic lesions, may progress to erythroderma in some patients. Pruritic papular eruption and eosinophilic folliculitis also presents with papular eruptions.
Nail and hair changes (graying and other pigmentary changes), photosensitive eruptions, and diffuse alopecia are noticed. Among sexually transmitted diseases, chancroid, syphilis in homosexual men, and lymphogranuloma venereum, are more commonly associated with AIDS. Syphilis coexisting with HIV creates special problems.
Treatment: Almost all cutaneous manifestations in HIV can be managed by the same modalities as in seronegative persons.
Neurological Manifestations
1. AIDS encephalopathy Infection of the CNS by HIV leads to encephalopathy (HIVE) which is also known by terms such as AIDS dementia complex, AIDS dementia, and HIV associated cognitive motor complex. HIVE is a late manifestation when there is a profound immune suppression with CD4 counts below 200 per cmm. HIVE is a subcortical dementia, caused by leukoencephalopathy typically emerging over the course of weeks and months. Typical complaints are slowing of reasoning, forgetfulness, difficulties concentrating, lack of energy and drive, mild depressive symptoms and emotional blunting.
Magnetic resonance imaging often shows patchy, diffuse, hyperintense and relatively symmetrical lesions in the white matter. These changes indicate leukoencephalopathy. HIV-associated myelopathy whose histopathological hallmarks are vacuoles, most prominent in the cervical and thoracic parts of the spinal cord, hence called vacuolar myelopathy
2. Progressive multifocal leukoencephalopathy (PML) is a severe demyelinating disease of the central nervous system predisposed to by AIDS. It is caused by JC virus (JCV), which is a polyoma virus found worldwide. The main focus of disease is the white matter of the cerebral hemispheres, but the cerebellum and in some cases the grey matter may also be affected. The median interval between the onset of the first symptoms and death was between 3 and 6 months. Patients usually die of secondary complications after being bedridden for many weeks. In addition to cognitive disorders, which may range from mild impairment of concentration to dementia, focal neurological deficits are very typical of PML.
Mono- and hemiparesis are observed most frequently, as well as defects of speech and vision. MRI usually shows asymmetrical high signal intensity lesions in T2-weighted imaging, hypointense in T1-weighted images. Usually they do not show gadolinium enhancement or mass effect. Non-involvement of the grey matter is characteristic. The lesions are almost always asymmetrical.
3. Cerebral toxoplasmosis almost always results from the reactivation of a latent infection with Toxoplasma gondii, Patients may present with seizure, headache or focal neurological deficits. Cerebral toxoplasmosis is extremely rare above a CD4 T cell count of 100/cmm. It should always be expected when the CD4 T cell counts fall below 100/cmm. A CT or MRI scan of the head should be performed promptly in all cases of focal neurological deficit. Ring enhancing lesions and solitary or multiple abcesses should suggest the infection. Up to 97 % of patients with cerebral toxoplasmosis have IgG antibodies, and therefore absence of these antibodies help to rule out toxoplasmosis.
4. Cryptococcal meningitis is more common in advanced immunodeficiency when the CD4 count is less than 200 cells per cmm. C. neoformans is transmited by droplet infection.
5. Primary CNS lymphomas are late complications of HIV infection, occurring in up to 10 % of AIDS patients. Almost all cases are EBV- associated. Neurological deficits occur depending on their location.
6. Peripheral neuropathy may complicate all stages of HIV infection. Acute inflammatory demyelinating polyneuropathy (AIDP) and Guillain-Barré syndrome (GBS) usually occur during seroconversion or during the latent stages of HIV infection. Chronic inflammatory demyelinating neuropathy, vasculitic neuropathy, distal symmetrical sensory polyneuropathy and drug induced neuropathies may occur are all reported.
7. Reactivation of CMV infection: When the CD4 count falls below 50/cmm reactivation of CMV infection can lead to retinitis. Any visual impairment occurring subacutely or acutely, such as blurred vision or floaters especially unilaterally should prompt immediate ophthalmological examination. Oral and/or intravitreal gancyclovir or valacyclovir will be useful if started early. Primary prophylaxis is not effective against CMV retinitis.
Cardiovascular System Involvement
Cardiovascular involvement is common in HIV-infected patients.
Pericardial diseases: Pericardial effusion, Pericarditis (viral, bacterial, fungal), neoplasms (Kaposi’s sarcoma, lymphoma).
Myocardial involvement: HIV-associated dilated cardiomyopathy, acute or chronic myocarditis, Kaposi’s sarcoma or lymphoma and adverse effects of antiretroviral drugs.
Endocardial involvement: Infective endocarditis—bacterial or fungal and nonbacterial thrombotic endocarditis
Vascular diseases: Arteriosclerosis, vasculitis, perivasculitis, pulmonary artery hypertension.
Other Miscellaneous Infections
Oroesophageal candidiasis: Candidias takes the form of extensive and persistent superficial lesions over the oropharynx, the buccal mucosa, tonsillar ring, tongue and the oesophagus. Candida esophagitis usually occurs with oropharyngeal involvement, but in about one third of the cases there may not be oral lesions. Esophagitis presents with odynophagia and retrosternal pain. Fluconazole therapy rapidly clears the infection.
MANAGEMENT OF HIV INFECTION
General measures: HIV infection should be confirmed beyond doubt by appropriate investigations. The immunological status is assessed by CD4 estimation. Severity of infection can be assessed by estimating the viral load using PCR test or other methods. The coexistence of opportunistic infections should be confirmed by investigations. Regular repetition of CD4 T-cell count and RNA viral load helps to assess the progress of the disease.
Antiretroviral therapy aims at bringing down the virus levels to undetectable levels, i.e. below 20 copies per ml with the presently available tests. This will ensure immune reconstitution with the return of CD4 counts above 200 per cmm. Symptom free survival is also prolonged.
Different groups of drugs are used. These include reverse transcriptase inhibitors, (RTIs) protease inhibitors (PIs) and entry inhibitors. The RTIs belong to two groups, the nucleotide and nucleoside RTIs (NtRTIs and NRTIs) and nonnucleoside RTIs (NNRTIs). The reverse transcriptase inhibitors block the transcription of DNA from viral RNA, without which the genetic material cannot be incorporated into the human DNA. The Protease inhibitors block the protease enzyme, effectively preventing the formation and release of new virions. The newly added class of fusion inhibitors blocks the virus fusion with the CD4 and other receptors on the cell membrane, thus preventing the entry of the virus into a new cell
PREVENTION
AIDS is though a dreaded disease is preventable too. Sex with a regular uninfected partner is the safest way to prevent HIV infection through sex. However condoms, if properly used offer almost complete protection against acquiring infection during natural sexual intercourse.
Strict screening of blood products for transfusion reduces the risk considerably. Transmission in parenteral drug abuse groups is tackled by supply of sterile syringes by governmental and other agencies. Other measures to reduce illicit use of habituating drugs include counselling, group therapy and legal measures to prevent drug trafficking. Transmission in hospital settings can be reduced by proper practice of universal (standard) precautions.