INFECTION – GENERAL INFORMATION (Types, Sources and Pathogenesis), PATHOGENESIS, APPROACH TO PATIENT WITH FEVER, SYSTEMIC RESPONSES AND LAB INVESTIGATIONS
INTRODUCTION
Microbes are abundant in nature, the vast majority of them harmless to man and many of them essential to life. They are mostly commensals and a few are pathogens. The organisms capable of establishing themselves and multiplying in hosts are called parasites, which may be commensals or pathogens. All our body surfaces have an indigenous bacterial flora. This normal flora protects us from infection by multiple mechanisms 1, compete with pathogens in utilizing nutrients. 2, producing antibacterial substances inhibiting growth of pathogens. 3, inducing host immunity that is cross reactive and effective against pathogens.
Pathogens lead to adverse effects on hosts while commensals cause no harm to their hosts and exist in harmony. Commensals may cause disease when host resistance is lost or when transferred to an inappropriate site, e.g. oropharyngeal commensals aspirated into lung.
Infection:
Infection is defined as multiplication of microbes in the tissues of the host with or without producing disease. Infections without disease manifestations are called subclinical infections.
Infections remain one of the main causes of morbidity and mortality in man worldwide. Poverty and overcrowding in the underdeveloped countries increase this burden. Infectious agents include bacteria, viruses, fungi, protozoa, helminths and prions.
Types of Infections
1. Exogenous infections: Infection from external source.
2. Endogenous infection: Infection by organisms harbored by the individual.
3. Primary infection: Initial infection of a host by an organism.
4. Secondary infection: Host suffering from an infectious disease invaded by another organism.
5. Re-infection: Subsequent infection by same organism.
6. Focal infection: Infections confined to one area/organ e.g. Tonsillitis.
7. Nosocomial infection: Infection acquired after admission to hospital.
8. Super infection: Patient receiving broad spectrum antibiotics get colonized by resistant pathogens and infection produced by them.
9. Opportunistic infection: Organisms that ordinarily do not cause infection in healthy individuals but do so in individuals with markedly reduced resistance (Immunocompromised hosts).
10. Latent infection: Pathogen remains in the tissue without producing disease but may lead to disease when host resistance is lowered.
Source of infection:
Infection may be obtained from human, animal or other sources. When the source of infection is man, the infectious agent may originate from patients or carriers.
A carrier who harbours the pathogenic organism without developing any disease due to it, is called healthy carrier.
A convalescent carrier is one who harbours the organism for some period after recovering from the disease.
Zoonoses are infections transmitted from wild or domestic animals to man e.g. plague, rabies.
Some infections are transmitted by insect vectors e.g. Anopheles mosquito transmits malaria.
Direct contact is necessary for transmission of organism like Staphylococci. Respiratory diseases such as influenza, tuberculosis, pneumonia and others spread by air-borne droplets. Food or Water borne transmission occurs in typhoid, hepatitis A and E, cholera and others. Sexual transmission is the main route for syphilis, gonorrhea and HIV. Vertical transmission i.e. from mother to fetus occurs in diseases like rubella and syphilis.
PATHOGENESIS
The pathological lesions, symptoms and signs may be produced by several mechanisms:
1. Caused by the organism directly e.g. Boils, abscesses, pneumonia, dysentery, tuberculosis.
2. Organisms like C. diphtheriae and Cl. tetani multiply locally without entering the system and elaborate toxins (exotoxins) which are absorbed into the system producing the manifestations.
3. Vibrio cholerae elaborates an exotoxin having local effect on the intestinal mucosa producing secretory diarrhea.
4. Many gram negative bacteria produce endotoxins by disintegration in the tissues producing direct effect on tissues and liberation of chemical mediators of inflammation like cytokines which are mainly responsible for the manifestations.
5. Activation of immunological mechanism is one of the most important pathogenic mechanisms of tissue damage in several infections.
6. Infections like HIV and syphilis suppress the immune mechanism of the host by acting upon the lymphocytes.
7. Some infectious agents are oncogenic i.e. giving rise to tumours- e.g. HIV, EB virus, hepatitis B and others. Medical care itself increases the patient’s risk of acquiring infection in several ways:
1. Contact with pathogens in the hospital.
2. Breach of skin (e.g. incisions, IV devices) or mucous membranes (e.g. endotracheal tube, indwelling catheter).
3. Alteration of normal flora by antibiotics.
4. Reduction of immunity by immunosuppressive drugs.
The body’s mechanisms to prevent and overcome the infections are local defenses, phagocytic cells, antibodies (immunoglobulins), immunocytes and nonspecific defense aids such as lysozymes, complement and properdin.
Changing scenario of infection worldwide: The pattern of infectious agents and pathogenesis are changing due to seceral factors such as changes in environment, influence of polymicrobial therapy and alterations in host defences.
Newly recognized infections are AIDS, severe acute respiratory distress syndrome (SARS), avian influenza and others.
Rebound of diseases like, malaria, tuberculosis, rheumatic fever and others thought to have been eradicated from developed countries. Recognition of role of infectious agents in the causation of diseases previously thought to be non-infectious e.g. Helicobacter pylori in the causation of peptic ulcer, Human papilloma virus in carcinoma cervix.
Human Polymicrobial Infections
In the immunocompetent state, colonization by one organism inhibits colonization by another. This is known as microbial interference e.g. S. pneumonia and S. aureus. At present, due to the prevalence of different kinds of immunosuppressed states, polymicrobial disease caused by combination of viruses, bacteria, fungi and parasites are being recognized. In this situation, presence of one micro-organism causes a niche for the other pathogen to colonize and thrive e.g. measles, tuberculosis and S.aureus; EB virus and retrovirus; HBV and HIV; HIV and tuberculosis.
Immunodeficiency states may be congenital or acquired. The latter include malnutrition, extremes of age, loss of surface epithelium, diabetes mellitus, cancer, cancer chemotherapy, chronic renal failure, chronic hepatic failure, immunosuppressant drugs, HIV infection and others. The resultant degree of immune suppression is the total effect of all the contributory factors. Immunodeficiency may be general or specific towards specific pathogens. Neutropenia and reduction of other phagocyte cells predispose to infection by extra cellular bacterial pathogens, both endogenous and exogenous. Suppression of T-cell mediated immunity predisposes to viral infections. Multiple intubations, hospitalization and management in intensive care facilities predispose to infections.
Clinical features of infection in the immunocompromised host differ from those in immunocompetent hosts. Signs of infection in the immunocompromised hosts include:
1. confusion
2. faint erythematous rashes
3. lymphangiectatic streaks on the skin
4. pleurisy dyspnoea or cough with clear chest X-ray
5. minimal erythema with serosanguineous discharge at sites of insertion of catheters, surgical sites, abscess or drains
6. minimally elevated values of liver function tests, and serum levels of LDH (lactic dehydrogenase) and C K (Creatine kinase) and
7. unexplained rise or fall of leukocytes and platelet counts.
Antimicrobial resistance:
As we developed newer antimicrobial drugs, microbes developed the ability to elude our best weapon. Antibiotic resistance is developing at an alarming rate. Multidrug resistant pathogens such as E. coli, Klebsiella, Pseudomonas, Staph. aureus, M.tuberculosis, HIV, and others are extremely common. Especially in the ICUs these get disseminated.
Bioterorrism:
Use of biological infectious agents such as anthrax spores, plague, small pox and others may be resorted to as potential weapons for stealthy warfare. Eradication of infectious diseases like smallpox totally from the world and polio from most countries has been achieved.
PATHOGENESIS OF FEVER
PATHOGENESIS
Pyrogens are substances causing fever. These may be exogenous or endogenous. Exogenous pyrogens are molecules which interact with host cells to induce secretion of pyrogenic cytokines. Most of these are microbial products, microbial toxins or whole microorganisms.
The best example is the lipopolysaccharide endotoxin found in the cell wall of gram-negative bacteria. Enterotoxin of S. aureus and Group A and B streptococci are other examples. Endogenous pyrogens are cytokines which are small molecular weight proteins most important being interleukin.1 (IL-1), IL-2 and tumour necrosis factor alpha (TNF α). The synthesis and release of pyrogenic cytokines are induced by a wide spectrum of exogenous pyrogens most of which are of bacterial, fungal or viral origin. In addition, inflammation, trauma, tissue necrosis and antigen–antibody complexes induce production of pyrogenic cytokines. Main source of pyrogenic cytokines are monocytes and macrophages, and to a lesser extent neutrophils and lymphocytes.
Pyrogenic cytokines stimulate production of the prostaglandin – PGE2 from arachidonic acid near the hypothalamic thermoregulatory centre. Arachidonic acid is released from cell membrane by the enzyme –Phospholipase A2. PGE2 raises the set point in the thermoregulatory center. Pyrogenic cytokines also induce production of PGE2 in the periphery which is responsible for myalgia, arthralgia and malaise that accompany fever.
Fever as a Defense Adaptation
There is suggestive evidence that, for some microorganisms at least, a febrile host response may assist in curtailing infection and speedy recovery. Experimental data support the notion that raised body temperature interferes with growth and / or virulence factors of some bacterial and viral pathogens. Fever, slightly increases immune reaction and increases chemotactic, phagocytic and bactericidal activity of polymorphonuclear leukocytes.
In immunocompromised individuals and those at the extremes of age, a prompt febrile response may notdevelop even in the presence of severe infection. Such persons are at greater risk of succumbing to the infection.
INFECTION – APPROACH TO PATIENT WITH FEVER
APPROACH TO PATIENT WITH FEVER
In the diagnosis of the cause of fever, science and art of Medicine come together. History is most important.
History of travel to a malaria – endemic area may give a clue. Presence of nasal symptoms and sore throat suggest viral etiology. Severe myalgia may suggest Influenza, Dengue fever or Leptospirosis. Eye congestion, subconjunctival hemorrhage and muscle tenderness may suggest leptospirosis. Skin rashes and mucous membrane lesions give diagnostic clue. Erythematous blanching rash indicates viral exanthematous fever as the most likely cause. Palatal petechiae along with posterior cervical lymphadenopathy and grey white tonsillar exudates suggests infectious mononucleosis. Enlarged tender tonsillar lymph nodes with tonsillar exudate and neutrophilic leukocytosis suggest streptococcal tonsillitis. Koplik’s spots in the buccal mucosa indicate measles. Dysuria and loin pain with tenderness suggests pyelonephritis.
Duration of Fever: This is an important point which helps in clinical diagnosis. Regular recording of temperature, pulse rate and respiration rate are routinely done in all hospitals. Fever of more than 5 to 7 days with gastro intestinal symptoms with or without malena and just palpable soft spleen may suggest typhoid fever. Onset may be abrupt in infections like pneumonia or may show a step-ladder type of rise in typhoid. Fever with clubbing of fingers and splinter hemorrhages in the nail bed in a patient with congenital or rheumatic valvular heart disease should suggest infective endocarditis.
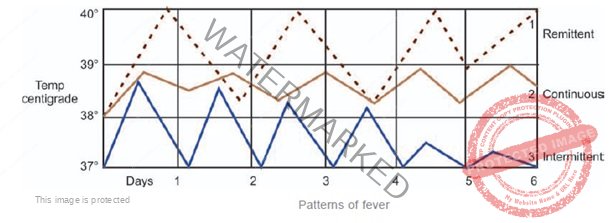
Patterns of Fever: Recording the pattern of temperature is an important clinical clue to diagnosis. In the ordinary febrile patient, temperature is recorded thrice daily, but in special cases where large fluctuations occur and in acute care settings temperature has to be recorded more frequently.
Continuous Fever Temperature is persistently elevated with diurnal variation of less than 1oC e.g. Typhoid in the 2nd week, typhus, viral infections and others.
Remittent Fever – Temperature is persistently elevated with diurnal variation more than 1oC – typhoid in 1st week, brucellosis, leptospirosis and others.
Intermittent Fever – Temperature is discontinuous, touching normal at least once in 24 hours. This may be seen in pyogenic infections, lymphomas, tuberculosis, bacteremias, malaria and others.
Periodic Fever: These show a regular periodicity in their occurrence. Fever occurring on alternate days with one day interval in between is called tertian periodicity e.g. vivax malaria (benign tertian). Fever occurring every 4th day with 2 days’ afebrile period in between is known as quartan periodicity e.g. quartan malaria. Continuous and remittent fevers may be converted to intermittent fever by repeated doses of antipyretics.
Drug Induced Fever Several drugs can produce fever by various mechanisms. These include allergy, systemic metabolic effects and agranulocytosis. Drug induced fever becomes a diagnostic problem in patients receiving multiple drugs for long periods, especially in hospitals.
Of the medications that cause fever, antibiotics are the most frequent–especially penicillins and cephalosporins, sulfonamides, nitrofurantoin, antituberculosis agents and others. Antiepileptic drugs especially phenytoin are also known to cause fever. Drug induced fever does not have specific characteristic features. Most often, it occurs 5 to 10 days after starting the drug, but can occur even after the first dose itself.
INFECTION – SYSTEMIC RESPONSES IN FEVER
SYSTEMIC RESPONSES IN FEVER
• Increase in metabolic rate – Oxygen consumption increases by 13% for each 1oC rise of temperature. Hence fever may aggravate or precipitate pre-existing cardiac, cerebrovascular or pulmonary insufficiency.
• Increase in heart rate. For every 1oC rise of temperature above normal, the heart rate increases by 18/minute. In some fevers like pneumonia and rheumatic fever, heart rate may be disproportionately high (rapid pulse fever). In typhoid, some viral infections, meningitis, brucellosis, drug induced fever and many cases of leptospirosis; pulse rate may be disproportionately slow (slow pulse fever).
• Blood pressure may increase during the period of rise of temperature because of vasoconstriction and decrease during the period of defervescence because of vasodilation.
• Fluid loss increases due to evaporation and sweating–average of 360 mL excess fluid is required for 24 hours for 1oC rise in temperature.
• Increase in respiratory rate occurs with fever. The usual ratio of 1:4 with heart rate is maintained except in the case of primary respiratory diseases such as pneumonia and pleural effusion.
• Chills occur in the initial phase because of peripheral vasoconstriction.
• Rigors accompany rapid increase in temperature. They are due to vigorous muscle contractions. Repeated occurrence of rigor is most typically seen in malaria, filariasis, urinary tract Infections, and abscess formation anywhere in the body. Rigor may occur in many types of continuous fever treated intermittently with antipyretics. When the effect of the drug wanes off rigor occurs in an attempt on the part of the body to resume the high temperature.
• When the high temperature falls to normal or subnormal within a few hours, it is called Fall by Crisis, and when the temperature reaches normal slowly over several days, it is called Fall by Lysis.
• Headache may accompany any type of fever but severe headache and photophobia are characteristic prominent features of intracranial infections and sinusitis.
• Delirium – This is toxic confusional state. It is more common in the very young and very old. Fever may induce mental changes in those with organic brain syndrome. The cytokines TNFα and IL-1 cause release of endorphins in the brain and may precipitate delirium.
• Excessive sweating is the regular accompaniment of defervescence. Particular patterns of sweating like “night sweats” are characteristic of tuberculosis and lymphoma. In almost all fevers fall of temperature is accompanied by sweating.
• Muscle pain – (myalgia) is characteristic of infections such as influenza, enterovirus, dengue fever, leptospirosis and others.
• Herpes labialis – Fever may activate the latent viral infection Herpes simplex which causes vesicles at muco-cutaneous junctions of the nose and lips. Pneumonia and meningitis are common to produce Herpes labialis whereas typhoid is very rare to do so.
• Feverishness: This is a subjective feeling of fever which may be experienced even without rise in temperature. Feverishness has not got the same pathological importance of fever. Therefore it is essential to record the temperature to distinguish between the two conditions.
INFECTION – FEVER OR INFECTION DETECTION – LAB INVESTIGATIONS
FEVER OR INFECTION DETECTION – LAB INVESTIGATIONS
Leukocyte Patterns
Neutrophil Leukocytosis and presence of juvenile or band forms of neutrophils and toxic granulations in neutrophils usually suggest bacterial infections. The severity of leukocytosis may also indicate the severity of sepsis. Total leukocyte counts above 10,000/cmm with more than 70% as neutrophils are very suggestive of pyogenic infection. Leukemoid reaction may accompany severe leukocytosis.
Neutropenia, mild to moderate, is usually seen in many viral infections, about 25%, of typhoid, brucellosis, leishmaniasis, tuberculosis, histoplasmosis and others.
Leukopenia with relative or absolute lymphocytosis occurs in several viral infections. Many viral infections show moderate or even severe thrombocytopenia with or without bleeding manifestations.
Atypical lymphocytes – are seen in some viral infections especially Epstein–Barr virus, cytomegalo virus, HIV, dengue, rubella, viral hepatitis, varicella and others.
Monocytosis is commonly seen in typhoid and tuberculosis.
Eosinophilia: Occurs in parasitic infections, filariasis, tropical pulmonary eosinophila and hypersensitivity to drugs.
1. Isolation or identification of the infective agent in blood/urine/body fluids/pus and tissues specimens
a. Culture: Proper collection of sample without contamination and transport to the lab is important e.g. blood culture in sepsis, urine culture in UTI, CSF in meningitis, sputum in pneumonia, pus in abscess.
b. Gram stain of specimen may help e.g. sputum, CSF, pus, urethral discharge and others. The findings on gram stain should correspond to the results of culture, to be diagnostic.
c. Demonstration of parasites like malaria and microfilaria in blood, leishmania in bone marrow and liver biopsy specimens, vegetative amoeba in stool or scrapings from abscess wall.
2. Demonstration of antibodies to specific pathogen e.g. Widal in typhoid, IgM antibodies against many viruses like hepatitis A, E and dengue virus.
3. Detection of bacterial/fungal/viral antigens in blood/body fluids even when cultures are negative or practically difficult e.g. HBsAg in virus B hepatitis.
4. Detection of very minute quantities of foreign nucleic acid by techniques such as PCR (polymerase chain reaction) that allow amplification of specific DNA/RNA sequences.
5. Histopathology: e.g. tuberculosis, histoplasmosis, sarcoidosis and others can be diagnosed by biopsy of lymph node, liver and other organs.


