PSYCHOPHARMACOTHERAPY – Principles of Psychopharmacologic Therapy, Purposes of Psychopharmacotherapy, Reasons for Non-compliance to Psychotropic Regimen, Services that Encourage Adherence to Medication Regimen, Effects on Special Populations and Safe Medication Administration: The Seven Rights (MENTAL HEALTH NURSING)
Psychopharmacologic agents (also called psychotropic or psychotherapeutic medications) are to relieve symptoms, but not “cure mental illness”. Clients taking psychotropic medications and their families need education regarding the medications action, purpose, intended effects, side effects, toxic or dangerous effects, treatment for side-effects and what to do about adverse or toxic effects. Non-adherence must be managed; client may not remember to take psychotropic medications or may refuse to take them at all or as prescribed. Medications may need to be changed and/or dosage adjusted in accordance with drug effectiveness and client response. Nurses must observe and document the client’s responses to and beliefs about medications
PRINCIPLES OF PSYCHOPHARMACOLOGIC THERAPY
- Psychopharmacologic agents do not “cure” mental illness
- Clients require physical and psychiatric assessments before psychotropic medication is prescribed for them
- Clients hold various views about the use of psychotropic medications; some of these views may bring about nonadherence to medication treatment
- Clients must give informed consent prior to administration of psychotropic medication including an explanation of risks versus benefits
- Psychotropic medication has different onsets of actions. Most medications (lithium, antidepressants) require daily administration for one to several weeks before their intended effects are evident; some medications (benzodiazepines, antipsychotics) act more immediately
PURPOSES OF PSYCHOPHARMACOTHERAPY
- Relieve or reduce symptoms of dysfunctional thoughts, moods, or actions, mental illness or disorder
- Improve client’s functioning
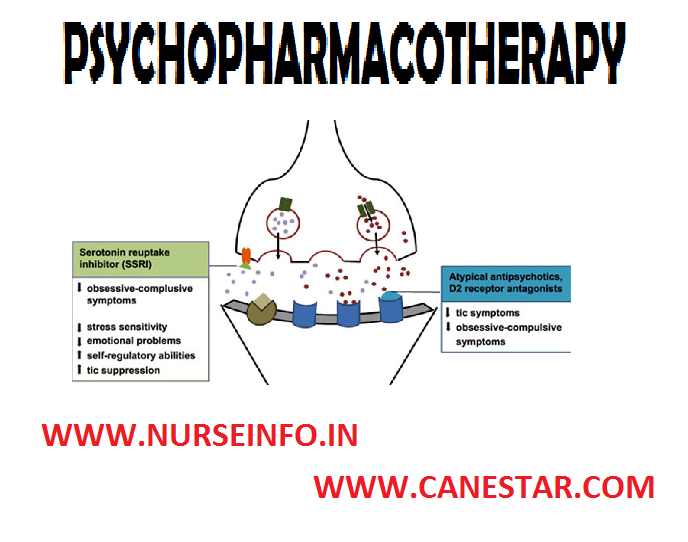
- Increase client’s adherence (or compliance) and amenability to other therapies. Most psychotropic medications act by modulating neurotransmitters (brain chemicals), specifically serotonin, norepinephrine (noradrenaline), dopamine, acetylcholine and glutamate
REASONS FOR NON-COMPLIANCE TO PSYCHOTROPIC REGIMEN
- Medications may be expensive and the client cannot afford them
- Clients may refuse to take medications because of their unpleasant or distressing side-effects
- Clients may stop taking their medications because they begin to feel better and believe that they no longer need the medications
- Clients may not believe they have any illness requiring medication or fear the stigma associated with having a mental illness and taking medication
- Mental illness itself such as paranoia, contributes to the client’s denial or fears about medication usage
SERVICES THAT ENCOURAGE ADHERENCE TO MEDICATION REGIMEN
Follow up interactions with the client will help the nurse verify that the client understands the purpose, proper administration, intended effects, side and toxic effects of, and how to treat serious problems associated with psychotropic medications
- Support persons can encourage and assist the client’s adherence to his or her psychotropic medication regimen
- Appropriate laboratory tests must be conducted to prevent serious complications and assure safe and therapeutic level of psychotropic medication
- Medication groups often provide not only education, but also peer support to those taking psychotropic medication. Often clients and their families have misconceptions that are preventing the client from taking his or her medication
- Depot injections (injections of medication into a body area where it will be deposited and stored) of antipsychotic medication can provide two or four weeks dosage of the medication to clients who have difficulty adhering to their medication schedule
EFFECTS ON SPECIAL POPULATIONS
Children: psychotropic medications should be administered with great caution to children. Initiating treatment with small dosages and increasing the dosages slowly diminishes the likelihood of side effects. Although the small volume of distribution suggests the use of lower doses than in adults, a child’s higher rate of metabolism suggest that a higher ratio of mg of drug to Kg of body weight should be used
Elderly: elderly clients are more susceptible to side effects, especially cardiac effects and may metabolize and excrete drugs more slowly
- Lower doses are needed for the elderly client because of decreased liver and renal function
- Elderly clients are likely to be taking other drugs; therefore, they have an increased risk for drug-drug interactions
- They may have decreased liver and renal function, therefore, their BUN (Blood, Urea, Nitrogen), creatinine, and liver enzymes should be monitored regularly
- Regular use of sedating medications for sleep should be discouraged because they usually return to normal sleeping patterns after only a few nights of medication use
- Discourage sedating medications as they may cause excessive sedation, confusion or disorientation resulting in falls and other injuries
Pregnancy: the basic rule is to avoid administering any drug to a woman who is pregnant (particularly during the first trimester) or who is breastfeeding a child. This rule however, occasionally needs to be broken when the mother’s psychiatric disorder is severe
BASIC PHARMACOLOGIC PRINCIPLES
- Pharmacokinetics: it refers to the movement of medication molecules in the body, including absorption, distribution, metabolism and excretion of medications
- Absorption: the movement of a medication from its site of administration (e.g. GI tract, muscle, skin or subcutaneous tissue) tissue to the bloodstream
- Distribution: the transportation of a medication to its site of action by bodily fluids
- Metabolism: occurs primarily in the liver. Individuals diagnosed with liver dysfunction have a increased ability to metabolize medications and are at risk of undue accumulation of medication and possible toxicity
- Excretion: the elimination of a medication from the body primarily through the kidneys. Individuals diagnosed with renal dysfunction should be monitored for an increase in duration and intensity of medication responses
- Medication responses: plasma medication levels can be regulated to control medication responses. Medication dosing attempts to maintain plasma levels between the minimum effective concentration (MEC) and the toxic concentration. When a medication has achieved plasma levels that are effective and not toxic, the plasma level is within the therapeutic range
- Therapeutic index (TI): medications with a high TI have a wide safety margin. Therefore, there is no need for routine serum medication level monitoring. Medications with a low TI should have serum medication level monitored closely. Monitor peak levels based on the route of administration. For example, an oral medication may have a peak of 1 to 3 hours after administration. Whereas, if the medication is given intravenously, the peak time might occur within 10 minutes
- Half-life: the plasma half-life is the time taken for the plasma concentration of the drug to decline to one-half of its value
- Pharmacodynamics (mechanism of action): describes the interactions between medication and target cell, body systems, and organs to produce effects. Medications interact with cells in one or two ways. Medications can mimic the receptor activity regulated by endogenous compounds or block normal receptor activity regulated by endogenous compounds. For example, morphine is classified as an agonist because it activates the receptors that produce analgesia, sedation, constipation and other effects
KEY POINTS/KNOWLEDGE REQUIRED PRIOR TO MEDICATION ADMINISTRATION
Medication category/class: medications may be organized according to pharmacologic action, therapeutic use, body system, chemical make-up, and safe use during pregnancy
Mechanism of action: this is how the medication produces the desired therapeutic effect
Therapeutic effect: this is the primary action for which the medication is administered to a specific client
Adverse effects: these are any unintended or undesired effect that can occur at a normal medication dose
Side effects: there are secondary medication effects that occur at therapeutic doses. These are usually predictable
Drug-drug interaction: some medications may be given together to increase or decrease the therapeutic effect. Two medications together may increase or decrease the adverse side effects
Drug food interaction: food may alter medication absorption and/or contain substances that react with certain medications
Toxicity: an adverse medication effect that is considered severe and may be life threatening. It can be caused by an excessive dose, but can occur at therapeutic dose levels
CONTRAINDICATION/PRECAUTIONS
- A specific medication can be contraindicated for a client based on the client’s condition. For example, a patient with history of allergy to a particular medication
- Precaution should be taken for a client who is more likely to have an adverse reaction than another client. For example, morphine depresses respiratory function, so it should be used with caution for clients who have impaired respiratory function
Preparation, dosage and administration: It is important to know any special consideration for preparation, recommended doses and how to administer the medication
Nursing implications: know how to monitor therapeutic effects prevent and treat adverse effects provide for comfort, and instruct clients in the safe use of medications
SAFE MEDICATION ADMINISTRATION: THE SEVEN RIGHTS
- Right client: verify the client’s identification each time a medication is given check identification band, name and/or photograph
- Right drug: correctly interpret medication order (verify completeness and clarity); read label three times; when container is selected, when removing dose from container, and when container is replaced; leave unit dose medication in its package until administration
- Right dose: calculate correct medication dose; check drug reference to ensure dose is within usual range
- Right time: give medication on time to maintain consistent therapeutic blood level. It is generally acceptable to give the medication ½ an hour before or after the scheduled time
- Right route: select the correct preparation for the ordered route. Know how to safely and correctly administer medication
- Right documentation: immediately records pertinent information, including client’s responses to the medication
- Right to refuse: clients have the right to refuse to take a medication. Determine the reason for refusal, provide information regarding risk for refusal, and notify appropriate health care personnel and document refusal and action taken