PERICARDITIS – Definition, Classification, Causes, Signs and Symptoms, Pathophysiology, Diagnostic Evaluations and Management
DEFINITION
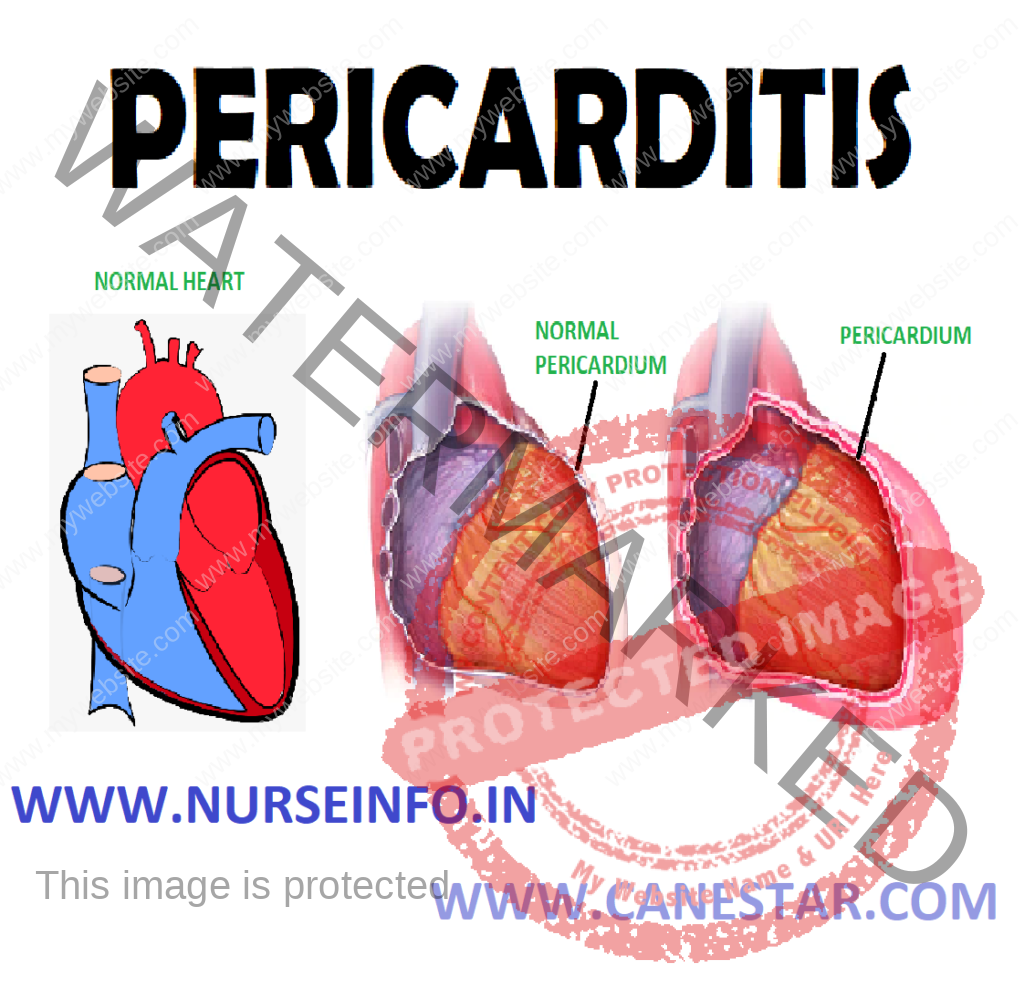
Pericarditis is an inflammation of the pericardium (the fibrous sac surrounding the heart)
- Pericarditis is inflammation of the pericardium, which causes its two layers to rasp and rub against each other as the heart contracts and relaxes
- Classification: it is of two types: (acute pericarditis, chronic pericarditis)
CLASSIFICATION ON THE BASIS OF ETIOLOGICAL FACTORS
- Acute nonspecific (idiopathic)
- Infective (bacterial, viral and other infections)
- Immunologic: (rheumatic fever, other connective tissue disorders)
- Neoplastic
- Metabolic (uremic, myxedema, gout)
- Traumatic (including after cardiac surgery)
- Associated with myocardial infarction
Infective
- Bacterial pericarditis: this condition is potentially fatal without prompt medical treatment. Most cases of bacterial pericarditis are triggered by infections somewhere else in the body. For example, a person with pneumonia (lung infection) may be vulnerable to bacterial pericarditis if the bacteria access the pericardium directly or via the bloodstream. Some of the dangerous complications include
Cardiac tamponade: fluid builds up between the two layers of the pericardium. The heart is compressed and cannot function properly
Abscess: a buildup of pus either within the heart or in the pericardium
Spread of infection: as with any infection, the infection can spread to other areas.
Constrictive pericarditis: the pericardium is scarred by the inflammation. Scar tissue does not stretch, so the heart cannot function properly
- Viral pericarditis: viral infections that cause cold or pneumonia, such as the echovirus or coxsackie virus (which are common in children) as well as influenza
Chronic effusive pericarditis: long-term inflammation causes a gradual buildup of fluid within the two layers of the pericardium. In most cases, the reasons for this are unknown. Some of the known causes of chronic effusive pericarditis include tuberculosis and hypothyroidism (underactive thyroid gland)
Constrictive pericarditis: as the pericardium recovers from injury or inflammation, scar tissue may form. Scar tissue makes the pericardium stiff and hard, so that the heart is unable to fill properly with blood. Symptoms include unexplained weight loss, fatigue, and breathlessness, swelling of the abdomen and heart murmurs. Without treatment, constrictive pericarditis can lead to a range of complications including:
Irregular heartbeat (heart arrhythmia)
Heart failure
Liver damage
- Neoplastic: cardiac myxoma, cardiac rhabdomyoma, papillary fibroelastoma, cardiac fibroma, cardiac lipoma, cardiac hemangioma, cardiac teratoma, mesothelioma of atrioventicular node, purkinje cell tumor
- Traumatic: heart surgery or trauma to the chest, esophagus or heart
- Pericarditis following heart surgery: pericarditis may be a complication of heart surgery. Operations on the heart involve opening the pericardium in order to apply coronary artery bypass grafts, open or replace heart valves, or undertake other corrective procedures
- Post heart attack pericarditis: while pericarditis does not cause or contribute to heart attack, the injury to cardiac tissue caused by a heart attack can sometimes lead to pericarditis. This is known as postmyocardial infarction (post-MI) pericarditis. The symptoms may not appear for some weeks or months after the heart attack, and can include relatively mild chest pain, joints pain and fever. It is not possible to prevent post-MI pericarditis
- Acute pericarditis: It is the inflammation of the pericardium characterized by chest pain, pericardial friction rub and serial of ECG changes (ST elevations)
Types include: pericarditis can be classified according to the composition of the inflammatory exudates
- Serous: this form usually consists of 50 to 200 ml of slowly accumulating exudates. Characteristically produced by nonbacterial involvement, including rheumatic fever, systemic lupus erythermatosus, tumors, uremia and primary viral infection (e.g. coxsackie)
- Purulent: this is due to bacteria, fungus or parasitic action. Infection reaches directly, through blood or through lymphatic route from the nearby areas of infection.
- Fibrinous: in this exudates will be completely resolved or be organized, causing adhesive pericarditis
- Caseous: this form is due to tuberculosis by direct extension from neighboring lymph nodes
- Hemorrhagic: this is composed of an exudates of blood mixed with fibrinous to suppurative effusion. Most commonly after cardiac surgeries
CAUSES
- Infectious: caused by viral, bacterial, fungal
Other:
- Idiopathic: no identifiable etiology found after routine testing
- Immunologic conditions including systemic lupus erythematosus (more common among women) or rheumatic fever
- Myocardial infarction (Dressler’s syndrome)
- Trauma to the heart, e.g. puncture, resulting in infection or inflammation
- Uremia (uremic pericarditis)
- Malignancy (as a paraneoplastic phenomenon)
- Side effects of some medications, e.g. isoniazide, cyclosporine, warfarin, and heparin
- Radiation-induced
- Aortic dissection
- Tetracycline
- Postpericardiotomy syndrome: usually after CABG surgery
PATHOPHYSIOLOGY
Migration of bacteria to pericardium and pericardial sac —– causes inflammation —- leading to chest pain, dry cough, fever, chills, fatigue, palpitation, anxiety, etc
SIGNS AND SYMPTOMS
- Chest pain
- Dry cough
- Fever
- Chills
- Fatigue
- Malaise
- Anxiety
- Joints pain
- Anorexia
- Increased heart rate (depends upon the degree of fever and anxiety)
- Weight loss
CHARACTERISTIC/PARAMETER: Pain description
PERICARDITIS: Sharp, pleuritic, retrosternal (under the sternum) or left precordial (left chest) pain
MYOCARDIAL INFARCTION: Crushing, pressure-like, heavy pain, described as ‘elephant on the chest’.
CHARACTERISTIC/PARAMETER: Radiation
PERICARDITIS: Pain radiates to the trapezius ridge (to the lowest portion of the scapula on the back) or no radiation
MYOCARDIAL INFARCTION: Pain radiates to the jaw, or the left arm, or does not radiate
CHARACTERISTIC/PARAMETER: Exertion
PERICARDITIS: Does not change the pain
MYOCARDIAL INFARCTION: Can increase the pain
CHARACTERISTIC/PARAMETER: Position
PERICARDITIS: Pain is worse in the supine position or upon inspiration (breathing in)
MYOCARDIAL INFARCTION: Not positional
CHARACTERISTIC/PARAMETER: Onset/duration
PERICARDITIS: Sudden pain that lasts for hours or sometimes days before a patient comes to the ER
MYOCARDIAL INFARCTION: Sudden or chronically worsening pain that can come and go in paroxysms or it can last for hours before the patient decides to come to the ER.
DIAGNOSTICS EVALUATIONS
- ECG: It indicates tachycardia but with underlying heart disease or uremia, bradycardia can occur
- Laboratory Investigation shows:
- Elevated ESR
- Elevated WBC cou t
- Cardiac enzymes are usually normal but may be elevated
- Physical Examination: It reveals the classical symptom, that is friction rub.
- Acute Complications: Pericarditis can progress to:
- Percardial effusion
- Cardia tamponade
- Pulsus paradoxus (decrease of at least 10 mm HG of the systolic blood pressure upon inspiration), hypotension (due to decreased cardiac index), JVD (jugular vein distention) from right-sided heart failure and fluid overload.
- Treatment: The treatment in viral or idiopathic pericarditis is with Aspirin, or non-steroidal anti-inflammatory drugs (NSAIDs, such as naproxen). Severe cases may require
- Antibiotics to treat tuberculosis or other bacterial causes.
- Steroids are used in acute pericarditis but are not favored because they increase the chance of recurrent pericarditis.
- Colchicine is a very effective treatment option. If aspirin and NSAIDs are not sufficient, colchicines should be added to the regimen.
SURGICAL MANAGEMENT
Pericardiocentesis is done to treat pericardial effusion/tamponade. (Pericardiocentesis is a procedure in which puncture of pericardial sac is done and some of the pericardial fluid is removed to relieve cardiac tamponade, which restricts normal heart action. During the procedure, the patient is monitored by ECG and central venous pressure measurements are made. A defibrillator is turned on and other emergency resuscitative equipment should be kept ready.