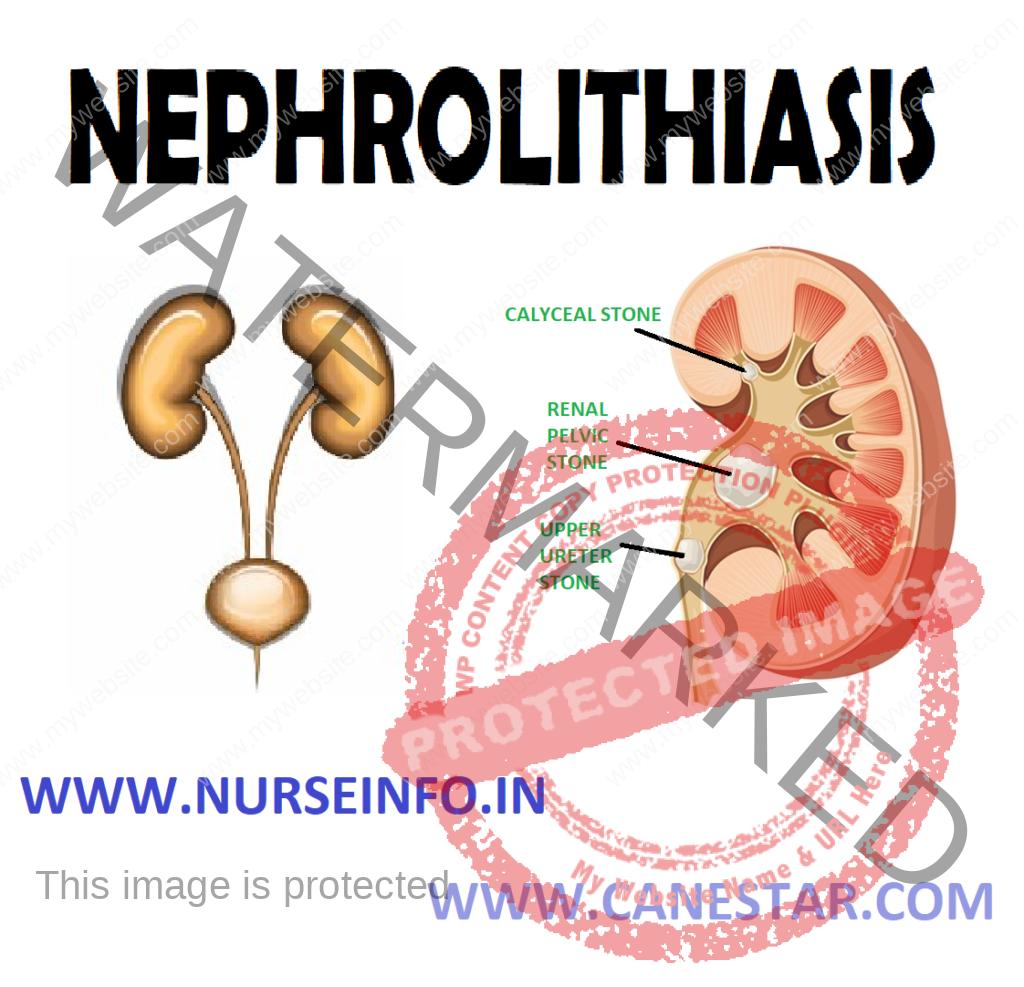
NEPHROLITHIASIS – Etiology, Risk Factors, Pathophysiology, Types, Signs and Symptoms, Diagnostic Evaluation and Management
Nephrolithiasis is also called the renal calculi, are hard, usually small stones that form somewhere in the renal structure. The stones are masses of crystals and protein that form when the urine became supersaturated with a salt capable of forming solid crystals.
Symptoms occur when the stone become impacted in the urinary tract. When stones are found in the kidneys, the condition is called nephrolithiasis.
ETIOLOGY
- Hypercalcemia and hypercalciuria caused by hyperparathyroidism
- Chronic dehydration, poor fluid intake and immobility
- Chronic infection with urea-splitting bacteria (proteus vulgaris)
- Chronic obstruction with stasis of urine, foreign bodies within the urinary tract
RISK FACTORS
- Metabolic: abnormalities that result in increased urine levels of calcium, oxaluric acid, uric acid or citric acid
- Climate: warm climate that cause increased fluid loss, low urine volume and increased solute concentration in the urine
- Diet
Large intake of dietary proteins that increases uric acid excretion
Excessive amounts of tea or fruit juices that elevate urinary level
Large intake of calcium and oxalate
Low fluid intake that increases urinary concentration
- Genetic factors: family history of stone formation, cystinuria, gout, or renal acidosis
- Lifestyle: sedentary occupation, immobility
PATHOPHYSIOLOGY
Due to any cause —- slow urine flow —- resulting supersaturation of the urine with the particular element —- first become crystallized —- later become stone
TYPES
- Calcium oxalate, calcium phosphate, or mixture
Incidence: 90%
Feature: account for two-third of stones. Small, rough, and hard. Shaped like needles, colors vary from gray to white
Possible causes:
Excessive calcium. Excessive urea. Hyperparathyroidism, Cushing’s disease, immobility, etc
Predisposing factors: idiopathic hypercalciuria, hyperoxaluria, independent of urinary pH, family history
- Struvite – magnesium ammonium phosphate
Incidence: 2%
Features: second most common type of stone. Calculi crumble easily. Stones have a yellow color
Causes: infection by urea splitting microbes, usually proteus. May cause abscess formation in the kidney
Predisposing factors: urinary tract infection
- Uric acid stones
Incidence: 2%
Features: dye enhancement needed for x-ray visualization. Small, hard and color varies from yellow to red
Causes: gout, high uric acid levels, decreased fluid intake
Predisposing factors: gout, acid urine, inherited condition
- Cystine stones:
Incidence: rare
Feature: small, smooth calculi, waxy stones
Causes: cystine-containing crystals appear in the urine
Predisposing factors: acid urine
SIGNS AND SYMPTOMS
- Costovertebral angle pain
- Groin pain
- Renal colic because renal stones produce an increase in hydrostatic pressure and distention of the renal pelvis and proximal ureters causing renal colic. Pain relief is immediate after stone passage
- Flank pain radiating to genitalia
- Hematuria
- Anuria
- Restlessness
- Pallor
- Temperature
- Nausea vomiting, diarrhea, abdominal discomfort due to renointestinal reflexes
DIAGNOSTIC EVALUATION
- History collection
- Physical examination
- Kidney radiography may show stone
- IVP (intravenous pyelogram), retrograde pyelogram is used to localize the degree and site of obstruction or to confirm the presence of a radiolucent stones, such as uric acid or cystine calculus
- Urinalysis: may indicate gross or microscopic hematuria and could indicate abrasion of the urinary tract
- Ultrasonography can be used to identify a radiopaque or radiolucent calculus in the renal pelvis, calyx, or proximal ureters. But it is less useful when attempting to locate stones trapped in the midureter
- A CT scan may be used to differentiate a non-opaque stone from the tumor
- Lab test: serum calcium, phosphorus, sodium, potassium, bicarbonate, uric acid, BUN and creatinine levels are also measured
MANAGEMENT
Medical Management
- The goals of management are to eradicate the stone, determine the stone type, prevent nephrons destruction, control infection, and relieve any obstruction that may be present
- The immediate objective of treatment of renal colic is to relieve the pain until its cause can be eliminated
- Opioid analgesic agents are administered to prevent shock and syncope that may result from the excruciating pain
- Nonsteroidal anti-inflammatory drugs (NSAIDs) are effective in treating renal stone pain because they provide specific pain relief. They also inhibit the synthesis of prostaglandin E, reducing swelling and facilitating passage of the stone
- Hot baths or moist heat to the flank areas may also be helpful
Nutritional Therapy
- Nutritional therapy plays an important role in preventing renal stones
- Fluid intake is the mainstay of most medical therapy for renal stones
- Patient with renal stones should drink eight to ten ounce glasses of water daily or have IV fluids prescribed to keep the urine dilute
- A urine output exceeding 2 L/day is advisable
International Procedures
If the stone does not pass spontaneously if complications occur, common intervention includes endoscopic or other procedure. For example:
- Ureteroscopy
- Extracorporeal shock wave lithotripsy (ESWL)
- Endourologic (percutaneous) stone removal
Ureteroscopy
- It involves first visualizing the stone and then destroying it
- In this inserting an ureteroscope into the ureter and then inserting a laser, electrohydraulic lithotripter, or ultrasound device through the ureteroscope to fragment and remove the stones
Extracorporeal shock wave lithotripsy
- It is used for most symptomatic, nonpassable upper urinary stones. Electromagnetically generated shock waves are focused over the area of the renal stone
- The high energy dry shock waves pass through the skin and fragment the stone
Endourologic (Percutaneous) stone removal
- It is used for most symptomatic, nonpassable, upper urinary stones. Electromagnetically generated shock waves are focused over the area of the renal stone
- The high energy dry shock waves pass through the skin and fragment the stone
Endourologic (Percutaneous) stone removal
- It is used to treat the larger stones
- A percutaneous tract is formed and a nephroscope is inserted through it. Then the stone extracted or pulverized
Electrohydraulic lithotripsy
- It is a similar method in which an electrical discharge is used to create a hydraulic shock wave to break up the stone
- A probe is passed through the cystoscope and the tip of lithotripter is placed near the stone
- This procedure is performed under topical anesthesia
- The most common complications are hemorrhage, infection and urinary extravasations
Chemolysis
- Stone dissolution using infusions of chemical solutions (e.g. alkylating agents, acidifying agents)
Surgical Management
- Today surgery is performed in only 1 to 2% of patients. It is indicated if the stone does not respond to other forms of treatment
- If the stone is in kidney, the surgery performed maybe a nephrolithotomy (incision into the kidney with removal of the stone) or a nephrectomy, if the kidney is nonfunctional secondary to infection
- Stones in the kidney pelvis are removed by pyelolithotomy
COMPLICATION
- Obstruction: from remaining stone fragments
- Infection: from dissemination of infected stone particles or bacteria resulting from obstruction
- Impaired renal function: from prolonged obstruction before treatment and removal
- Perirenal hematoma: from bleeding around the kidney caused by trauma of shock waves or laser treatments
Nursing Management
Nursing Assessment
- Obtain history focusing on family history of calculi, episodes of dehydration, prolonged immobility, UTI, dietary, bleeding history, and medication history
- Assess pain location and radiation; assess level of pain using a scale of 1 to 10. Observe for presence of associated symptoms nausea, vomiting, diarrhea, abdominal distension
- Monitor for signs and symptoms of UTI, such as chills, fever, dysuria, frequency. Examine urine for hematuria
- Observe for signs and symptoms of obstruction, such as frequent urination of small amounts, oliguria, anuria
Nursing Diagnosis
- Acute pain related to the presence of, obstruction or movement of a stone with in urinary system
- Impaired urinary elimination related to blockage of urine flow by stones
- Risk for infection related to obstruction of urine flow and instrumentation during treatment
- Anxiety related to hospitalization
- Fear related to deficient knowledge regarding the disease
- Deficient knowledge related to lack of knowledge about prevention of recurrence, diet and symptoms of renal calculi
- Acute pain related in the presence of obstruction or movement of a stone with in urinary system
Interventions
- Ask severity, location and duration of pain using a pain scale. Pain is typically in the flank or costovertebral angle and may radiate to the pelvic, groin, or abdominal area
- Encourage fluid intake, unless contraindicated, to promote the passage of stone, dilute the urine, and reduce the risk of further stone formation
- Administer pain medication as ordered to promote comfort
- Apply heat to flank pain area to reduce pain and promote comfort
- Impaired urinary elimination related to blockage of urine flow by stones
Interventions
- Monitor total urine output and pattern of voiding. Report oliguria or anuria
- For outpatient treatment, patient may use a coffee filter to strain urine
- Help patient to walk, if possible because ambulation may help move the stone through the urinary tract
- Teach patient to drink eight ounces of liquid with meals, between meals and in early evening to provide fluids for hydration but not to an excess that may increase renal colic
- Risk for infection related to obstruction of urine flow and instrumentation during treatment
Interventions
- Administer parenteral or oral antibiotics, as prescribed during treatment, and monitor for adverse effects
- Assess urine for color, cloudiness, and odor
- Obtain vital signs, and monitor for fever and symptoms of impending sepsis (tachycardia, hypotension)
Health Education
- Encourage fluids to accelerate passing of stone particles
- Teach about analgesics that still may be necessary for colicky pain, which may accompany passage of stone debris
- Warn that some blood may appear in urine for several weeks
- Encourage frequent walking to assist in passage of stone fragments
- Teach patient to strain urine through a coffee filter or stone strainer and to save for analysis
- Teach patient to take alpha-adrenergic blockers to help dilate ureters, thus improve stone passage