DIABETES MELLITUS – Types, Signs and Symptoms, Diagnostic Evaluation and Management
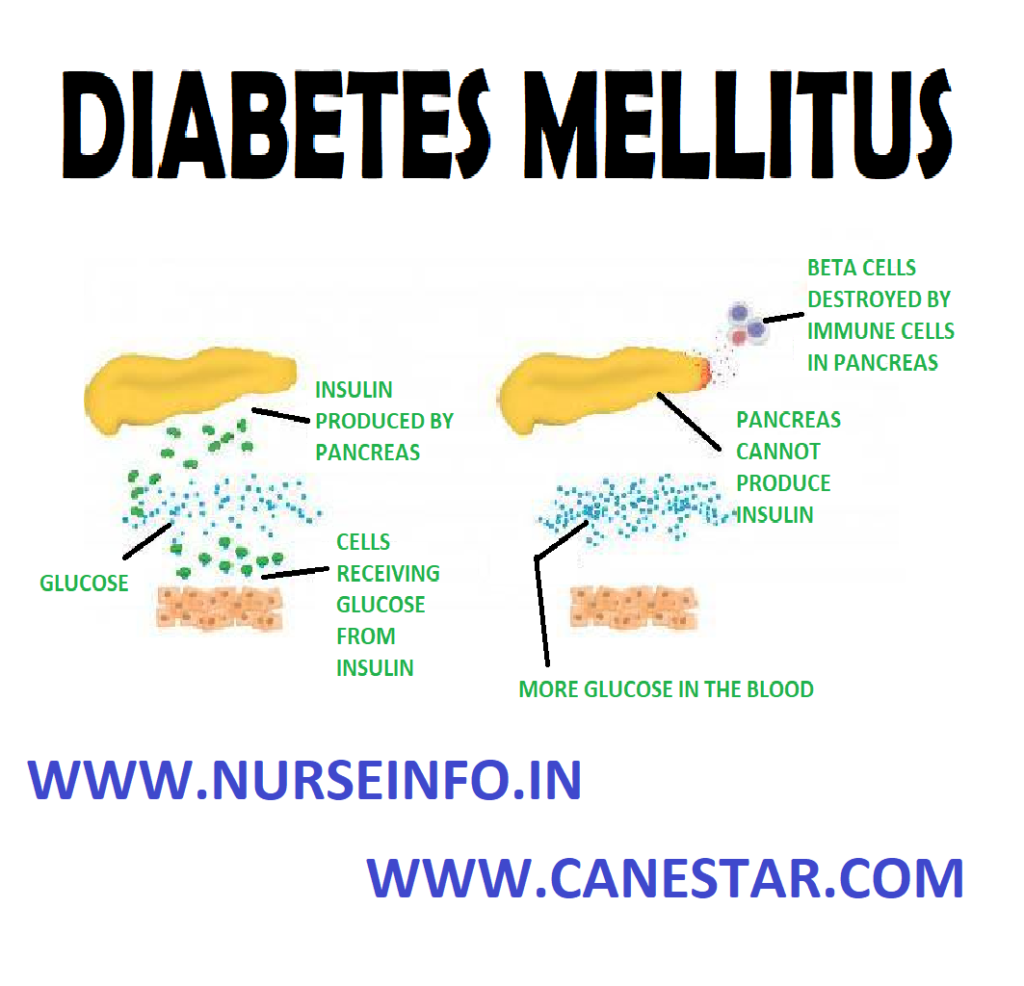
Diabetes mellitus is a group of metabolic diseases in which a person has high blood sugar, either because the pancreas does not produce enough insulin, or because cells do not respond to the insulin that is produced. This high blood sugar produces the classical symptoms of polyuria (frequent urination), polydipsia (increased thirst) and polyphagia (increased hunger). Hyperglycemia does not cause symptoms until glucose values are significantly elevated-above 200 milligrams per deciliter (mg/dL).
Diabetes mellitus is a group of chronic disorder of endocrine pancreas. This disease characterized by increased levels of glucose in blood (hyperglycemia) resulting from defects in insulin secretion, insulin action, both.
There are three main types of diabetes mellitus (Type-1 DM)
- TYPE-1 Diabetes Mellitus: Type 1 DM results from the body’s failure to produce insulin, and currently requires the person to inject insulin or wear an insulin pump. It is also called ‘insulin-dependent diabetes mellitus’ (IDDM) or ‘juvenile diabetes’. The immune system mistakenly manufactures antibodies and inflammatory cells that are directed against and cause damage to patients’ own body tissues. In persons with type 1 diabetes, the beta cells of the pancreas, which are responsible for insulin production, are attacked by the misdirected immune system. Exposure to certain viral infections (mumps and coxsackie viruses) or other environmental toxins may serve to trigger abnormal antibody responses that cause damage to the pancreas cells where is made. Some of the antibodies seen in type 1 diabetes include anti-islet cell antibodies, anti-insulin antibodies and anti-glutamic decarboxylase antibodies
- TYPE-2 Diabetes mellitus: Type 2 DM results from insulin resistance, also referred to as non-insulin-dependent diabetes mellitus (NIDDM) or ‘adult-onset diabetes.’ In type 2 diabetes, patients can still produce insulin, but do so relatively inadequately for their body’s needs. In many cases the pancreas produces larger than normal quantities of insulin. A major feature of type 2 diabetes is a lack of sensitivity to insulin by the cells of the body (particularly fat and muscle cells)
- Gestational diabetes: gestational diabetes, occurs when pregnant women without a previous diagnosis of diabetes develop a high blood glucose level. Gestational diabetes (or gestational diabetes mellitus, GDM) is a condition in which women without previously diagnosed diabetes exhibit high blood glucose levels during pregnancy (especially during their third trimester)
SIGNS AND SYMPTOMS
- Increased thirst (polydepsia)
- Frequent urination (polyuria)
- Increased hunger (polyphagia)
- Weight loss
- Fatigue
- Blurred vision
- Slow-healing sores or frequent infections
- Dark skin
DIAGNOSTIC EVALUATION
- Glycated hemoglobin test: this blood test indicates average blood sugar for the past two to three months. It measures the percentage of blood sugar attached to hemoglobin, the oxygen-carrying protein in red blood cells. A normal level is below 5.7 percent
- Random blood sugar test: a blood sample will be taken at a random time. Regardless of when you last ate, a random blood sugar level of 200 mg/dL (11.1 mmmol/L) or higher suggests diabetes, a blood sugar level less than 140 mg/dL (7.8 mmol/L) is normal.
- Fasting blood sugar test: a blood sample will be taken after an overnight fast. A fasting blood sugar level from 100 to 125 mg/dL (5.6 to 6.9 mmol/L) is considered prediabetes. If it is 126 mg/dL (7 mmol/L) or higher on two separate tests, indicates diabetes.
- Oral glucose tolerance test: it is rarely used test for hyperglycemia, patient is asked to fast overnight, and the fasting blood sugar level is measured. Then drink a sugary liquid, and blood sugar levels are tested periodically for the next two hours. A blood sugar level less than 140 mg/dL (7.8 mmol/L) is normal. A reading of more than 200 mg/dL (11.1 mmol/L) after two hours indicates diabetes. A reading between 140 and 199 mg/dL (7.8 mmol/L and 11.0 mmol/L) indicates prediabetes.
- Urine glucose and ketone levels: these are not as accurate in monitoring, changes in blood glucose as serum or blood levels. The presence of glucose in urine indicates hyperglycemia.
COMPLICATIONS
- Cardiovascular disease
- Nerve damage (neuropathy)
- Kidney damage (nephropathy) or kidney failure
- Damage to the blood vessels of the retina (diabetic retinopathy), potentially leading to blindness
- Clouding of the normally clear lens (cataract)
- Feet problems caused by damaged nerves or poor blood flow that can lead to serious infections
- Bone and joint problems, such as osteoporosis
- Skin problems, including bacterial infections, fungal infections and non healing wounds
- Teeth and gum infections
- Dawn phenomenon: It is rise of blood glucose between 4 am to 8 am that is not a response to hypoglycemia. This condition occurs in people both DM1 and DM2. Cause is unknown but due to hormone variation.
- Diabetic ketoacidosis: diabetic ketoacidosis develops when there is too little insulin in body. Without enough insulin, sugar cannot enter in cells for energy. Blood sugar level rises and body begins to break down fat for energy. This process produces toxic acids known as ketones. Excess ketones accumulate in the blood and eventually ‘spill over’ into the urine. Diabetic ketoacidosis can lead to diabetic coma that can be life-threatening.
- Diabetic hyperosmolar syndrome: this condition occurs when production of insulin is normal, but it does not work properly. Blood glucose levels may become very high-greater than 600 mg/dL (33 mmol/L). Because insulin is present but not working properly, the body cannot use either glucose or fat for energy. Glucose is then dumped in the urine, causing increased urination. If left untreated, diabetic hyperosmolar syndrome can lead to coma and life-threatening dehydration
MANAGEMENT
Nutritional Therapy
Nutrition, meal planning and weight control are the foundation of diabetes management.
The main objective is to control dietary caloric intake to maintain normal weight. Medical nutrition therapy (MNT), nutritional management of diabetes is complex, a registered dietician who understand dietary management has major responsibilities for designing and teaching aspect of therapeutic plan.
Regular blood sugar monitoring
Regular exercise
Regular diabetes medication or insulin therapy
Alcohol: alcohol and the substances use to make mixed drinks can cause either high or low blood sugar
Stress: the hormones body may produce in response to prolonged stress may prevent insulin from working properly
For women, fluctuations in hormone levels: as hormone levels fluctuate during menstrual cycle, so cans blood sugar level also, particularly in the week before period. Menopause may trigger fluctuations in blood sugar level as well
Pharmacological Management
- Biguanides
- Sulfonylureas
- Meglitinide derivatives
- Alphaglucosidase inhibitors
- Thiazolidinediones (TZDs)
- Glucagon like peptide-1 (GLP-1) agonists
- Dipeptidyl peptidase IV (DPP-4) inhibitors
- Selective sodium-glucose transporter-2 (SGLT-2) inhibitors
- Insulins
- Amylinomimetics
- Bile acid sequestrants
- Dopamine agonists
Insulin Therapy
Some people who have type 2 diabetes need insulin therapy as well. Because normal digestion interferes with insulin taken by mouth, insulin must be injected. Insulin injections involve using a fine needle and syringe or an insulin pen injector – a device that looks like an ink pen, except the cartridge is filled with insulin
Types of insulin are many and include rapid-acting insulin, long-acting insulin and intermediate options. Examples include:
- Insulin lispro (Humalog)
- Insulin aspart (Novolog)
- Insulin glargine (Lantus)
- Insulin detemir (Levemir)
- Insulin isophane (Humulin N, Novolin N)
Life Style and Home Remedies
- Commit to managing your diabetes: Make healthy eating and physical activity part of your daily routine. Establish a relationship with a diabetes educator, and ask your diabetes treatment team for help when you need it
- Wear a tag or bracelet that says you have diabetes. Keep a glucagon kit nearby in case of a low blood sugar emergency and make sure your friends and loved ones know how to use it.
- Schedule a yearly physical exam and regular eye exams
- Keep your immunizations up-to-date. Get a flu shot every year, and get a tetanus booster shot every 10 years
- Take care of your teeth. Diabetes may leave you prone to gum infections. Brush your teeth at least twice a day, floss your teeth once a day, and schedule dental exams at least twice a year
- Pay attention to your feet. Wash your feet daily in lukewarm water. Dry them gently, especially between the toes and moisturize with lotion. Check your feet everyday for blisters, cuts, sores, redness or swelling
- Keep your blood pressure and cholesterol under control
- Quit smoking
- If you drink alcohol, do so responsibly
- Take stress seriously
NURSING MANAGEMENT
Nursing Diagnosis
- Fluid volume deficit related to osmotic diuresis, gastric loss, excessive diarrhea, nausea and vomiting, limited input
Intervention
- Monitor vital signs, note the presence of orthostatic blood pressure
- Assess breathing and breathe patterns
- Assess temperature, color and moisture
- Assess peripheral pulses, capillary refill, skin turgor and mucous membranes
- Monitor intake output. Record the urine specific gravity
- Measure body weight everyday
- Collaboration fluid therapy as indicated
- Imbalanced nutrition, less than body requirements related to insulin insufficiency.
Intervention
- Measure body weight per day as indicated
- Determine the diet program and diet of patients compared with food that can be spent on the patient
- Auscultation of bowel sounds, record the presence of abdominal pain/abdominal bloating, nausea, vomiting, keep fasting as indicated
- Observation of the signs of hypoglycemia, such as changes in level of consciousness, cold/humid, rapid pulse, hunger and dizziness
- Collaboration in the delivery of insulin, blood sugar tests and diet.
- Risk for infection related to inadequate peripheral defense, changes in circulation and high blood sugar levels
Intervention
- Observation for signs of infection and inflammation such as fever, redness, pus in the wound, purulent sputum, urine color cloudy and foggy
- Increase prevention efforts by performing good handwashing, each contact on all items related to the patient, including his or her own patients
- Maintain aseptic technique in invasive procedures(such as infusion catheter foley, etc)
- Attach catheter/perineal care do well
- Give skin care with regular and earnest. Massage depressed bone area, keep skin dry, dry linen and tight (not wrinkled)
- Position the patient in semifowler position
- Collaboration antibiotics as indicated
- Knowledge deficit: About condition, prognosis and treatment needs related to misinterpretation of information; do not know the source of information
Intervention
- Assess the level of knowledge of the client and family about the disease
- Give an explanation to the client about diseases and conditions now
- Encourage clients and families to pay attention to her diet
- Ask the client and reiterated family of materials that have been given


Thanks for the information
Thanks for information
Thnq so much 🥰😍