GASTRIC ANALYSIS – Basal Gastric Analysis (Tube), Stimulation Gastric Analysis (Tube), Tubeless Gastric Analysis, Normal Findings, Purpose, Clinical Problems, Client Preparation, Procedure, Tubeless Gastric Analysis and Factor Affecting Diagnostic Results
The gastric analysis test examines the acidity of the gastric secretions in the basal state (without stimulation) and the maximal secretory ability (with stimulation, i.e. with histamine phosphate, betazole hydrochloride (histalog) indicate a peptic ulcer (stomach or duodenal), and an absence of a HCl (achlorhydria) could indicate gastric atrophy (possibly caused by gastric malignancy) or pernicious anemia.
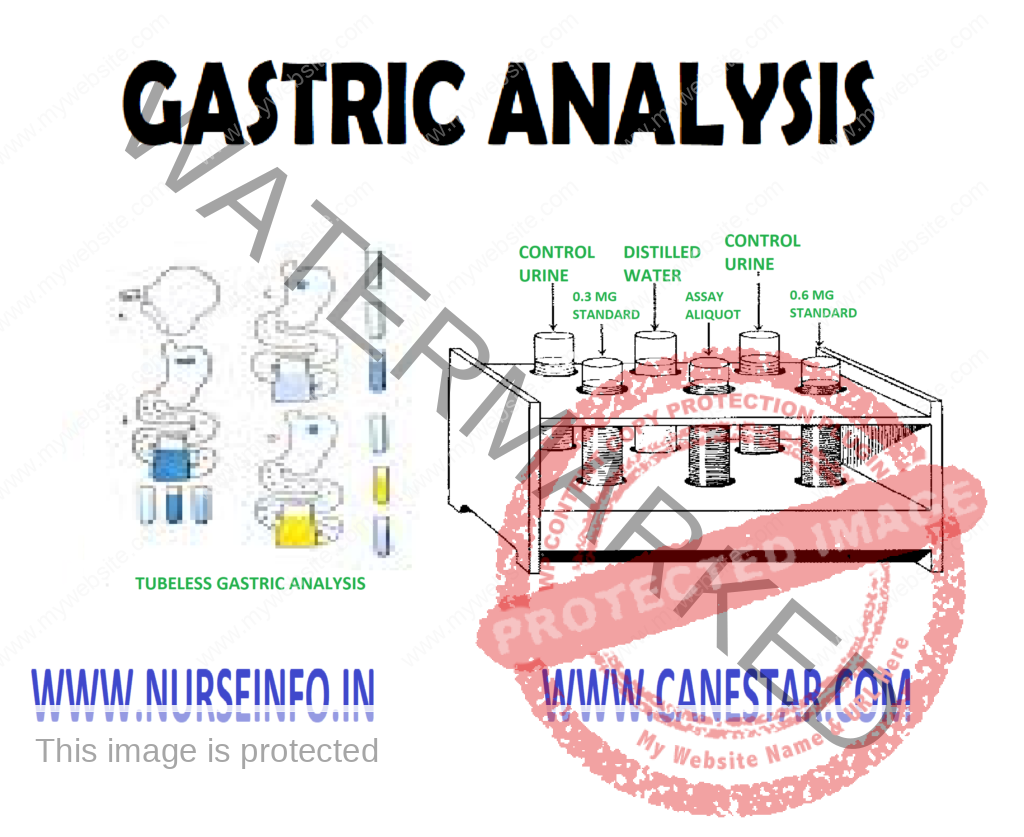
In addition, gastric contents can be collected for cytological examinations. Gastric analysis by tube (basal and stimulation) and tubeless gastric analysis (urine examination after a resin dye and stimulant are administered) are the methods used for evaluating gastric secretions.
BASAL GASTRIC ANALYSIS (TUBE)
Gastric secretions are aspirated through a nasogastric tube after a period of fasting. Specimens are obtained to evaluate the basal acidity of the gastric content first and the gastric stimulation test follows.
STIMULATION GASTRIC ANALYSIS (TUBE)
The stimulation test is usually a continuation of the basal gastric analysis. After samples of gastric secretions are obtained, a gastric stimulant (i.e. histalog or pentagastrin) is administered, and gastric contents are aspirated every 15 – 20 minutes until several samples are obtained.
TUBELESS GASTRIC ANALYSIS
This test is for screening purpose to detect the presence or absence of HCl; however, it will not indicate the amount of the free acid in the stomach. A gastric stimulant (caffeine, histalog) is given, and an hour later a resin dye (azuresin, diagnex blue) is taken orally by the client. The free HCl releases the dye from the resin base; the dye is absorbed by the gastrointestinal tract and is excreted in the urine. Absence of the dye in the urine after 2 hours is indicative of gastric achlorhydria. This test method saves the client discomfort of being intubated with nasogastric tub; however, it does lack accuracy.
NORMAL FINDINGS
- Fasting: 1.0-1.5 mEq/L/h
- Stimulation: 10-25 mEq/L/h
- Tubeless: detectable dyes in the urine
PURPOSE
- To evaluate gastric secretions
- To detect an increase or decrease of free HCl
CLINICAL PROBLEMS
Decreased Level
- Pernicious anemia
- Gastric malignancy (atrophy)
- Atrophic gastritis
Elevated Level
- Peptic ulcer (duodenal)
- Zollinger-Ellison syndrome
CLIENT PREPARATION
- Explain the purpose and procedure of the tube or tubeless gastric analysis test to the client. Check with the healthcare providers before you give your explanation to find out whether he or she will perform both basal and stimulation gastric analysis. List the steps of the test on paper for the client, if needed.
- Tell the client how the nasogastric tube is inserted (i.e. the tube is lubricated and passes through the nose or mouth) and that he or she will be asked to swallow or will be given sips of water as the tube is passed into the stomach. The end of the tube may be attached to low intermittent suction
- Notify the healthcare provider if the client is receiving the following categories of drugs; antacids, antispasmodics, anticholinergics, adrenergic blocker, cholinergics and steroids. Drugs from the above groups and a few others should be withheld for 24-48 hours before the gastric analysis. Drugs that cannot be withheld should be listed on the request slip.
- Monitor vital signs. Observe for possible side effects for use of stimulants (i.e. dizziness, flushing, tachycardia, headache and a lower systolic blood pressure)
- Label the specimens (gastric or urine) with the client’s name, the date, the time and the specimen’s number
- Be supportive of the client. Encourage the client to express his or her concerns or fear. Answer questions or refer to appropriate health professions
PROCEDURE
- The client should be on NPO for 8 hours to 12 hours prior to the test. Smoking should be restricted for hours
- Certain groups (i.e. anticholinergics, cholinergics, adrenergic blockers, antacid, and steroids) and alcohol and coffee should be restricted for atleast 24 hours before the test. It should be notes on the request slip if the drugs cannot be withheld.
- Baseline vital signs should be recorded
- Loose dentures should be removed
- A lubricated nasogastric tube is inserted through the nose or mouth
- A residual gastric specimen and four additional specimen taken 15 minutes apart should be aspirated and labeled with the client’s name, the time, and a specimen number. The nasogastric tube may be attached to low intermittent suction
Stimulation Test
A continuation of the basal gastric analysis
- A gastric stimulant is administered (i.e. betazole hydrochloride (histalog) or histamine phosphate intramuscularly; pentagastrin subcutaneously)
- Several gastric specimens are obtained over a period of 1-2 hours (histamine four 15-minute specimens in 1 hour and histalog eight 15-minute specimen in 2 hours). Specimens should be labeled with the client’s name, the date, the time, and specimen numbers.
- Vital signs should be monitored. Emergency drugs, such as epinephrine (adrenalin) should be available
- The test usually takes 2 and half hours for both parts (basal and stimulation)
TUBELESS GASTRIC ANALYSIS
- The client should be on NPO for 8-12 hours before the test
- The morning urine specimen is discarded
- Certain drugs are withheld for 48 hours before the test (i.e. antacids, quinine, iron, vitamin B complex), with the health care providers permission
- Give the client caffeine sodium benzoate 500 mg in a glass of water
- Collect a urine specimen 1 hour later. This is control urine specimen
- Give the client the resin dye agent (azuresin or diagnex blue) in a glass of water
- Collect a urine specimen 2 hours later. The urine may be colored blue or blue green for several days. Absence of color in the urine usually shows absence of HCl in the stomach
FACTORS AFFECTING DIAGNOSTIC RESULTS
- Incorrect labeling of specimens could affect test results
- Drugs: antacids, anticholinergics, and histamine blockers (cimetidine, ranitidine) could decrease HCl levels; antacids, electrolyte and iron preparations, vitamin B complex, and quinidine could fastly elevate the diagnex blue level
- Stress, smoking and sensory stimulation could increase HCl secretions


It’s amazing essay for study