CHOLANGIOGRAPHY (INTRAVENOUS, PERCUTANEOUS, T-TUBE) – Description, Clinical Problem, Client Preparation and Procedure
DESCRIPTION
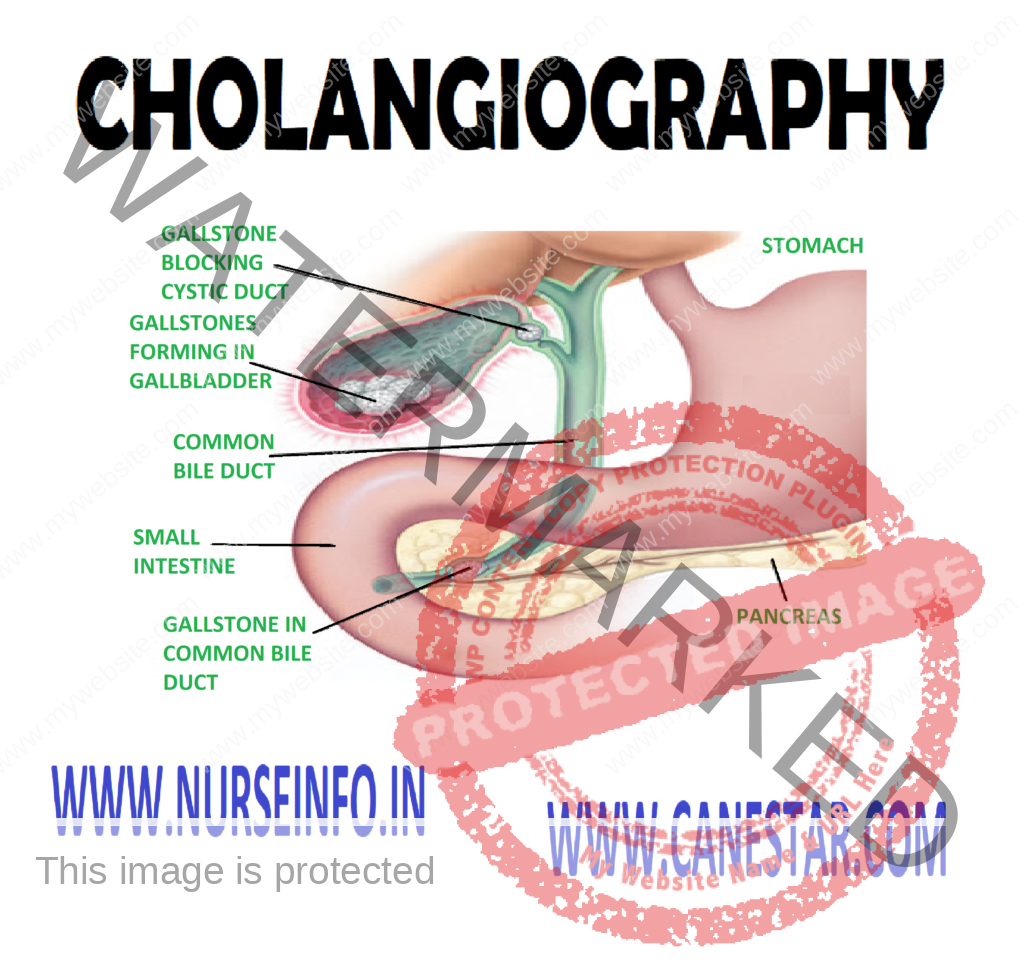
Intravenous (IV) cholangiography examines the biliary ducts (hepatic ducts within the liver, the common hepatic duct, the cystic duct, and the common bile duct) by radiographic and tomographic visualization. Often the gallbladder is not well-visualized.
The contrast substances, an iodine preparation such as iodipamide meglumine (cholografin) are injected intravenously. Approximately 15 minutes, X-rays are taken. IV cholangiography is a tedious and time consuming test, and reactions are more common with the IV contrast substances than with the oral agents.
Percutaneous cholangiography is indicated when biliary obstruction is suspected. The contrast substances are directly instilled into the biliary tree. The process is visualized by fluoroscopy and spot films are taken.
T-tube cholangiography is also known as postoperative cholangiography may be done 7-8 hours after a cholecystectomy to explore the common bile duct for patency of the duct and to see if any gallstones are left. During the operation, a T-shaped tube is placed in the common bile ducts to promote drainage. The contrast substances are injected into the T-tube. A stone or two could be missed during a cholecystectomy, causing occlusion of the duct.
- Normal findings: patient biliary ducts (absence of stones and strictures)
CLINICAL PROBLEM
Test
- IV cholangiography
Indications: to detect stricture, stones, or tumor in the biliary system
- Percutaneous cholangiography
Indications: to detect obstruction of the biliary system caused from stones, cancer of pancreas
- T-tube cholangiography
Indications: to detect obstruction of the common bile duct from stones or stricture, fistula
CLIENT PREPARATION
- Explain the client the purpose and procedure for the IV cholangiography, percutaneous cholangiography or T-tube cholangiography
- Check with your institution to see if procedure differ and make modifications in your explanation to the client
- Explain the procedure step by step for the client, as requested. This can decrease high levels of anxiety
- Obtain a client history of allergies to sea food, iodine or X-ray dye. Report a history of allergies to these substances to the healthcare provider, and record in the client’s chart
- Permit the client to express his or her concerns. Answer questions, if possible
- Check that consent form has been signed by the client before giving a sedative and before the test
- Administer the pre-test orders (e.g. laxatives, sedatives, etc)
- Inform the client having IV cholangiography that the test may take several hours (up to 4 hours)
- Observe for signs and symptoms allergic reaction to contrast agents (e.g. nausea, vomiting, flushing, rash, urticaria, hypotension, slurred, thick speech and dyspnea)
- Check the infusion site for signs of phlebitis (e.g. pain, redness, and swelling). Apply warm compresses to the infusion site if symptoms are present, as ordered
- Check the vital signs as ordered following the percutaneous cholangiography
PROCEDURE
IV Cholangiography
- A consent form for IV cholangiography should be signed
- The client should be on NPO for 8 hours the test. Some radiologist encourages fat-free liquids before the test to prevent renal toxicity caused by the injected dye
- A laxative (e.g. citrate of magnesium or castor oil) maybe given the night before the test, and cleansing enema may be given in the morning. Keeping the gastrointestinal tract clear can prevent shadows in the X-ray films. Check with radiology department for the exact preparation needed
- A contrast agent, iodipamide meglumine (cholografin) is injected intravenously while the client is lying on a tilting X-ray are taken every 15-30 minutes until the common bile duct is visualized
Percutaneous Cholangiography
- A consent form for percutenous cholangiography should be signed
- The client should be on NPO for 8 hours before the test
- A laxative the night before and cleansing enema the morning of the test may be ordered
- Preoperative medications usually include sedatives/tranquilizers. An antibiotic may be ordered for 24-72 hours before the test for prophylactic purposes
- The client is placed on tiling table that rotates. The upper right quadrant of the abdomen is cleaned and draped. A local (skin) anesthetic is given
- The client should exhale and hold his or her breath while a needle is inserted with the guidance of fluoroscopy into the biliary tree. Bile is withdrawn, and the contrast substances are then injected. Spot films are taken
- A sterile dressing is applied to the punctured site
T-tube Cholangiography
- A consent form for T-tube cholangiography should signed
- The client should be on NPO for 8 hours before the test
- A cleansing enema may be ordered in the morning before the test
- The client lies on an X-ray table, and a contrast agent such as sodium diatrizoate (hypaque) is injected into the T-tube and an X-ray is taken 15 minutes later
- The T-tube may be removed after the procedure or it may be left in place
Factors affecting diagnostic results: obesity and gas or fecal material in the intestines can affect the clarity of the X-ray
Client education: instruct the client to remain in bed or 6 hours following percutaneous cholangiography