COPD (Chronic Obstructive Pulmonary Disease) CHRONIC BRONCHITIS – General Characteristics, Pathogenesis, Pathology, Clinical Features, Diagnosis and Management
General Characteristics
Chronic bronchitis is defined as a disease characterized by hypersecretion of mucus sufficient to cause cough and sputum on most days for at least three months in a year for two or more consecutive years. This happens in the absence of any other specific respiratory or cardiovascular disease.
In the initial stages the inflammation of the bronchi is intermittent and recurrent, later it becomes established. The larger air passages are affected during the early part of the disease, later obstructive features set in when the smaller airways are also affected. Infection leads to periodic aggravation of the symptoms and the sputum, which is mucoid, becomes purulent during these episodes. As the airways obstruction progresses, emphysema sets in. These two processes become established in the majority of cases so that the condition is termed chronic bronchitis emphysema syndrome (CBES). The disease is more common in damp, cold, and dusty regions. Atmospheric pollution is accompanied by a higher incidence of CBES.
COPD (Chronic Obstructive Pulmonary Disease)
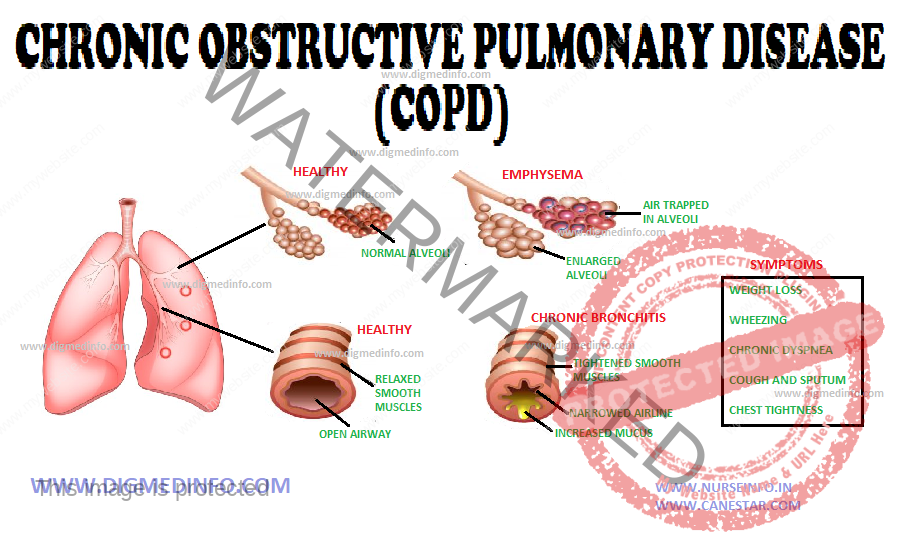
Chronic Obstructive Pulmonary Disease (COPD) is a major cause of chronic morbidity and mortality throughout the world. Chronic Obstructive Pulmonary Disease (COPD) is a disease state characterized by airflow limitation that is not fully reversible. The airflow limitation is usually both progressive and associated with an abnormal inflammatory response of the lungs to noxious particles or gases.
The most important risk factor for COPD is cigarette smoking. Pipe, cigar and other types of tobacco smoking popular in many countries are also risk factors for COPD. Passive exposure to cigarette smoke also contributes to respiratory symptoms and COPD.
Other documented causes of COPD include occupational dusts and chemicals (vapours, irritants, and fumes) when the exposures are sufficiently intense or prolonged. Indoor air pollution from biomass fuel used for cooking and heating in poorly ventilated dwellings. Outdoor air pollution, which adds to the lungs total burden of inhaled particles, although its specific role in causing COPD isnot well understood.
Symptoms of COPD include:
Cough
Sputum production
Dyspnea on exertion
Episodes of acute worsening of these symptoms often occur. Chronic cough and sputum production often precede the development of airflow limitation by many years; although not all individuals with cough and sputum production go on to develop COPD.
Pathogenesis
Chronic obstructive pulmonary disease (COPD) is a descriptive term given to the syndrome seen mostly in the elderly, who have airflow obstruction, not completely relieved by therapy. At least three distinct pathological processes may occur concurrently or separately in different subjects lead to COPD.
These are:
1. Emphysema which is due to destruction of alveolar walls
2. Chronic bronchitis with hypersecretion of mucus, and 3. Asthma with airway remodeling.
COPD encompases chronic obstructive bronchitis with obstruction of small airways and emphysema with enlargement of air spaces, destruction of lung parenchyma, loss of lung elasticity and closure of small airways. The inflammatory process in COPD differs from that in asthma in several ways. The type of inflammatory cells, inflammatory mediators, final outcome and response to treatment are different. In COPD the inflammation affects the peripheral airways-the bronchioles. The cells are macrophages, CD8 lymphocytes and neutrophils. The lung parenchyma is affected. Unlike as in asthma there is no preponderance of eosinophils.
Oxidative stress also plays a significant role in the pathogenesis. Even though the lungs bear the main brunt of the disease, systemic effects also occur. Muscle weakness and wasting may develop as part of the systemic disorder.
Pathology:
The bronchial mucosa shows hypertrophy and increase of the mucous glands and goblet cells with consequent overproduction of viscid mucus. The distal airways show narrowing of lumen caused by increased height of the epithelium and increased thickness of the muscle and connective tissue. The mucosa becomes ulcerated and when the ulcers heal, fibrosis occurs resulting in distortion of the lumen with stenosis and dilatation.
Distortion of the airways leads to permanent obstruction. Secondary infection occurs in the later stages. The ciliary movement is further impaired by the abnormally viscid mucus. This aggravates infection and a vicious cycle is established. Severe recurrent infections cause the development of microabscesses in the bronchial wall. These heal with fibrosis. Squamous metaplasia occurs. Distortion and obstruction of the bronchial lumen result in air trapping and emphysema of the alveoli, some show collapse and fibrosis.
The main pathological process can be summarized as follows:
1. Inflammation of the bronchi with enlargement of mucous glands and smooth muscle hyperplasia, all leading to wall thickening
2. Acinar distension due to the destruction of lung parenchyma probably mediated by imbalance of protease-antiprotease (alpha-1 antitrypsin) enzymes causing loss of support of small airways
3. Fibrosis and narrowing of the airways leading to increase in airway resistance.
The capillary bed is distorted and truncated and this aggravates the progression of pulmonary arterial hypertension. The pulmonary arteries become distended and atheromatous. Pulmonary hypertension gives rise to right ventricular hypertrophy and dilatation. Chronic cor pulmonale supervenes as time passes.
CLINICAL FEATURES
The clinical picture is varied depending on the severity and duration. The most frequent early symptom is cough recurring year after year, especially so in winter months. Later the cough becomes constant. Expectoration is mucoid and the sputum is tenacious, especially on waking up in the morning. Main complaint is the feeling of tightness of the chest. Physical examination reveals mild wheeze which disappears as the patient clears the bronchi by expectoration. Variable degrees of bilateral rhonchi and coarse crepitations are heard as adventitious sounds.
Initially acute infections give rise to fever and purulent sputum. As the infection becomes established, fever and other general symptoms come down. At this stage the quantity and character of the sputum are more reliable indicators of infection. The sputum becomes copious in amount when bronchiectatic changes develop. With the development of emphysema the chest assumes the inspiratory position and the respiratory excursions are considerably diminished. At this stage dyspnea is far out of proportion to the physical findings in the chest.
Key Indicators for Considering the Diagnosis of COPD
Chronic cough: Present intermittently or every day. Often present throughout the day; seldom only nocturnal
Chronic sputum production: Any pattern of chronic sputum production may indicate COPD
Acute bronchitis: Repeated episodes
Dyspnea that is: Progressive (worsens over time), Persistent (present every day), Worse on exercise, Worse during respiratory infections
History of exposure to risk factors: Tobacco smoke (including popular local preparations), Occupational dusts and chemicals and smoke from home cooking and heating fuel
DIAGNOSIS
Chronic bronchitis should be diagnosed from the history of recurrent cough extending over several years, mucopurulent sputum and the physical findings of bronchial obstruction and emphysema. X-ray is normal in the early stages but the features of emphysema may be evident later. X-ray may be helpful in identifying precipitating conditions like pneumonia, pneumothorax during the time of an exacerbation. HRCT is useful in quantifying the severity of emphysematous changes and locating areas with bronchiectatic changes.
Lung function tests show reduction in vital capacity, increase in the closing volume and features of airway obstruction. Based on the spirometry values severity of obstruction can be categorised as mild, moderate severe and very severe.
Differential diagnosis:
Chronic bronchitis has to be distinguished from asthma. Differentiation is easy in the early stages but there is considerable overlap of symptoms and signs in the advanced stages, and, therefore, the clinical assessment is difficult.
Other conditions like pulmonary tuberculosis, bronchiectasis, heart failure and bronchogenic carcinoma, obliterative bronchiolitis, diffuse pan bronchiolitis have to be ruled out in atypical cases.
Course and prognosis: Established chronic bronchitis is incurable. Over several years the condition progresses to produce complications and death. Each infective exacerbation leads to further deterioration in lung function and precipitates the development of respiratory failure and cor pulmonale. Exacerbation can occur as a result of bacterial infection of the lower respiratory passages, viral infections of the respiratory tract or due to non-infective causes such as environmental allergens and pollutants.
Complications: These include:
1. Frequent respiratory infections,
2. Respiratory failure, and
3. Right-sided heart failure (cor pulmonale).
MANAGEMENT
General measures: Most effective single step to prevent deterioration is to stop smoking. This single measure itself affords considerable relief of symptoms. Environmental allergens and pollutants must be avoided by the patient.
Other general measures include improvement in general health, regular exercise, deep-breathing exercises, adequate sleep, treatment of obesity, and eradication of foci of sepsis in the throat, nose and paranasal sinuses. If these measures are started during the early phase of the disease, further progression can be arrested.
Drugs: Apart from the general measures, no active treatment is indicated in the early stages.
Treatment
Treatment of infective episodes: A broad spectrum antibiotic should be employed for 7-10 days during an infective episode. Tetracycline or ampicillin may be started initially. Depending on the microbiological tests, the antibiotic may have to be changed.
Bronchospasm has to be relieved by the use of bronchodilators such as aminophylline, salbutamol or any other β-agonist. Ipratropium bromide is an anticholinergic muscarine receptor blocker, which blocks vagal reflexes responsible for bronchoconstriction. It is indicated when bronchospasm is troublesome.
Ipratropium bromide delivered by a metered dose inhaler in a dose of 40-80 μg helps to relieve bronchospasm without appreciable side effects. In COPD response of the airways to ipratropium is excellent. Tiotropium is a newer analogue which is equally effective.
Inhibitors of inflammatory response: Since inflammation plays a major role in the pathogenesis of COPD newer pharmacological agents are under trial. These include mediator antagonists which are capable of counteracting the effects of leukotrienes, lipoxygenases, interleukin B, tumor necrosis factor and the like. Protease inhibitors which inhibit neutrophil elastases, cathepsin and anti-inflammatory agents such as phosphodiesterase inhibitors are all in the process of development.
Several newer drugs especially phosphodiesterase-4 inhibitors are under trial. Roflumilast is a drug of this class given in a dose on 250 or 500 mg orally daily for 24 weeks. Results are encouraging.
Use of N-acetyl cysteine or bromhexine hydrochloride 8 mg thrice daily orally helps to liquefy the sputum. Steam inhalations help to improve vital capacity, relieve emphysema and open up the airways by expectorating the sputum.
Nonpharmacological measures: Noninvasive positive pressure ventilation and oxygen therapy at home using a simple nasal mask which eliminates the need for endotracheal intubation is beneficial. Long-term oxygen therapy has shown improved survival with better quality of life.
Pulmonary rehabilitation: Structured programme of education and exercises is very effective. Blowing into an air pillow repeatedly for 10-15 times twice a day and bending over a pillow held firmly on to the abdomen, in order to push the diaphragm up during expiration are simple maneuvers which can be practised at home.
Management of chronic respiratory failure: When hypoxemia becomes severe, i.e. PaO2 below 55 mm Hg or SaO2 below 80% at rest, continuous oxygen inhalation may have to be instituted for at least 18 hours a day. Oxygen therapy helps to reduce pulmonary arterial tension and allay cor pulmonale. In intractable cases lung transplantation may have to be considered.
Lung volume reduction surgery (LVRS): This has been found to be useful in selected cases. The rationale for this technique is to reduce the volume of over inflated emphysematous lung by 20-30%, in order to improve the elastic recoil of the lungs, to improve the configuration of the diaphragm, chest wall mechanics and gas exchange.
Lung transplantation: This procedure is in vogue for more than a decade in advanced countries.
Transplantation of a single lung or both heart and lungs as a whole is possible. Transplantation should be considered if the recipient is below 55 years of age, and is free from underlying conditions such as advanced diabetes, malignancy, hepatic or renal failure and conditions which impair mechanics of the chest wall. The donor should be ABO and HLA compatible with normal lungs, preferably between 12 and 50 years of age and with normal cardiopulmonary anatomy. Usually cadaver lungs are used for transplantation. Complications may occur as in the case of any other major organ transplantation.
Indications
1. Incurable respiratory failure—chronic or acute due to pulmonary causes
2. Irreversible structural and functional abnormalities in the lung such as fibrosis, extensive bronchiectasis, cystic disease, emphysema and others.