CHRONIC PERICARDITIS – Types, Causes, Pathophysiology, Diagnostic Evaluation, Clinical Features, Treatment and Management
DEFINITION
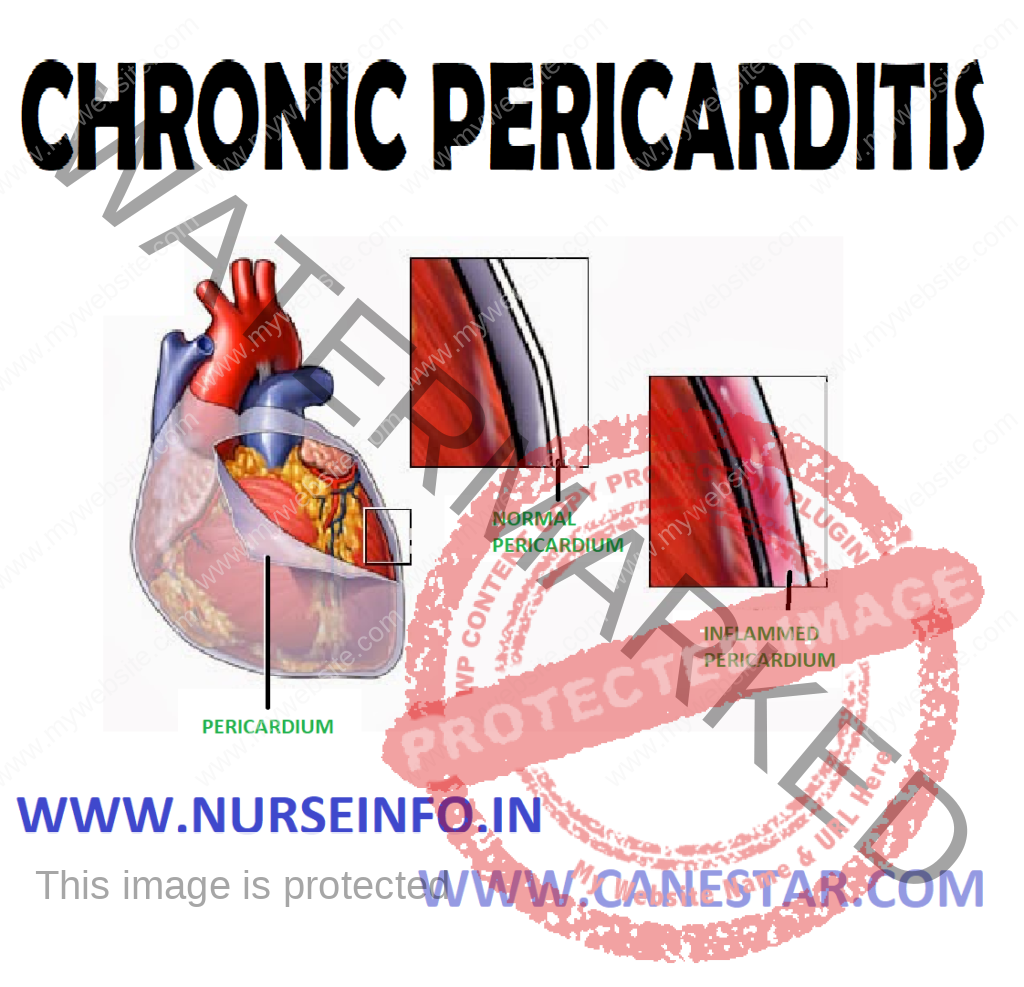
Chronic pericarditis is a condition in which there is chronic inflammatory thickening of the pericardium that changes the pericardium into thick fibrous band of tissues. Thus, the tissues encircle, encase and compress the heart and prevent it from expanding to normal size, causing restriction of ventricular filling.
TYPES
- Adhesive pericarditis
- Adhesive mediastinopericariditis
- Constrictive pericarditis
- Adhesive pericarditis: chronic pericarditis with adhesions between visceral and parietal pericardium
CAUSES
- Shortness of breath
- Pain: it may be steady and constant or it may occur in paroxysms, usually after unusual effort or after mental excitement or a fit of anger
- Pulse: rapid and feasible; pulse tension and pressure greatly reduced; irregular pulse
- Palpitations
- Ventricles become dilated and hypertrophied with its concomitant symptoms – dropsy, vertigo and venous stasis are present
- Treatment: it needs most careful and continuous oversight. Effusion should be retarded and its absorption and removal should be promoted by rational measures
- Adhesive mediastino pericarditis: here pericardial sac is obliterated due to adhesion between two layers of pericardium as well as between parietal pericardium and surrounding mediastinal structures, chest wall and diaphragm
- Constrictive pericarditis: constrictive pericarditis is a late sequela of an inflammatory condition of the pericardium. The inflammatory condition is usually an infection that involves the pericardium, but it may also occur after a heart attack or after heart surgery
Almost half the cases of constrictive pericarditis in the developing world are idiopathic in origin. In regions where tuberculosis is common, it is the cause in a large portion of cases. Causes of constrictive pericarditis include:
- Infectious (tuberculosis, incomplete drainage of purulent pericarditis, fungal and parasitic infections)
- Inflammatory and autoimmune: (chronic pericarditis, postviral pericarditis, postsurgical, following pericarditis associated with acute myocardial infarction, following postmyocardial infarction (Dressler’s) syndrome, in association with pulmonary asbestosis
- Prior mediastinal radiation therapy
- Chronic renal failure
- Connective tissue disorders
- Neoplastic pericardial infiltration
PATHOPHYSIOLOGY
Constrictive pericarditis is due to a thickened, fibrotic pericardium that forms a noncompliant shell around the heart —- this shell prevents the heart from expanding when blood enters it —-
- During inspiration, the negative pressure in the thoracic cavity will cause increased blood flow into the right ventricle —- increased volume in the right ventricle will cause the interventricular septum to bulge towards the left ventricle, leading to decreased filling of the left ventricle —- due to the Frank-Starling law, this will cause decreased pressure generated by the left ventricle during systole —- thi is known as ventricular interdependence since the amount of blood flow into one ventricle is dependent on the amount of blood flow into the other ventricle
- During expiration, the amount of blood entering the right ventricle will decrease —- allowing the interventicular septum to bulge towards the right ventricle, and increased filling of the left ventricle and subsequent increased pressure generated by the left ventricle during systole —- this is known as ventricular interdependence since the amount of blood flow into one ventricle is dependent on the amount of blood flow into the other ventricle
DIAGNOSTIC EVALUATION
- Imaging will demonstrate a thickened pericardium. In contrast with restrictive cardiomyopathy, there is an increased resistance to ventricular filling due to increased myocardial stiffness. Imaging features of restrictive cardiomyopathy demonstrate an increased left ventricular thickness with infiltration of the myocardium
- Chest X-ray: pericardial calcification, and pleural effusions are common findings
- Echocardiography: the echographic finding is an exaggerated anterior motion of the septum with the atrial filling. Since the posterior ventricular wall is unable to expand, an increase in left ventricular volume with the atrial systole produces a marked displacement of the septum
- CT and MRI: useful in select cases
- BNP blood test: tests for the existence of the cardiac hormone, brain natriuretic peptide which is only present in RCMP but not in CP, and is particularly helpful in determining the specific CHF type
- Pulmonary catheterization showed all four heart chambers having equal diastolic pressures
CLINICAL FEATURES
- Kussmaul’s sign (raised JVP on inspiration)
- Increased JVP (almost universal), rapid descent (prominent diastolic collapse of JVP)
- Pericardial knock in around 50% cases
- Hepatomegaly and other signs of right heart failure; ascites; fatigue; peripheral edema
TREATMENT
Pericardial stripping: the definitive treatment for constrictive pericarditis is pericardial stripping, which is a surgical procedure where the entire pericardium is peeled away from the heart. This procedure has significant risk involved, with mortality rates of 6%. The high risk of the procedure is attributed to adherence of the thickened pericardium to the myocardium and coronary arteries. In patients who have undergone coronary artery bypass surgery with pericardial stripping, there is danger of tearing a bypass graft while removing the pericardium. Due to the significant risks involved with pericardial stripping, many patients are treated medically, with judicious use of diuretics
Common Causes of Chronic Pericarditis
- Long-standing pyogenic infections
- Postviral infections
- Tuberculosis
- Hemopericardium
Common Signs and Symptoms of Chronic Pericarditis
- Congestive heart failure
- Dyspnea
- Chronic atrial fibrillation
- Fatigue on exertion
- Leg edema
- Ascites
- Low pulse pressure
- Distended neck pain
- Delay in capillary refill time
Common Treatment of Chronic Pericarditis
- Medical Treatment: digitalis and diuretics
- Surgical Treatment: surgical removal of the tough encasing pericardium (pericardiectomy) is the only treatment of benefit. The objective of the operation is to release both ventricles from the constrictive and restrictive inflammation. Surgery may be considered if the pericardium is scarred and inflexible, or if pericarditis keeps recurring.
- The procedure begins when the surgeon makes and incision in the skin over the breastbone and divides it to expose the pericardium. During the surgery, the surgeon will grasp the pericardium, cut the drop of this fibrous covering of the heart, drop it into the specimen bag, and re-cover the heart. The breastbone is then wired back together and the incision is closed, completing the procedure. When the portion of pericardium lying between the two phrenic nerves is excised, it is called total pericardiectomy. In cases where total pericardiectomy is not possible, subtotal pericardiectomy is performed or, in extreme cases, a cruciate incision on the pericardium is performed.
Nursing Management
Assessment
- Assess signs of pain
- Assess association of pain with respiratory movements, cough, swallowing
- Assess for pericardial friction rub (helps to distinguish between pericarditis and MI).
- Frequently check client for temperature (pericarditis can cause abrupt onset of fever in a previously afebrile patient).
Nursing Diagnosis
- Acute pain related to inflammation of layers of heart
Goal: to relieve pain
Interventions
- Check the intensity of pain
- Assist the patient to sit upright or to lean forward to relieve pain
- Restrict the activities of patient
- Provide prescribed analgesics (morphine).
- Hyperthermia related to inflammatory process
Goal: to maintain normal temperature
Interventions
- Monitor temperature 2-4 hourly
- Observe for basic principles of asepsis like handwashing
- Provide cold compression if chills are not present along with fever
- Administer prescribed antibiotics and antipyretics (decreased cardiac output related to structural abnormality of valves
Goal: to reduce risk of complications
Interventions
- Monitor BP and pulse (pulsus alternans indicates left-sided heart failure)
- Evaluate jugular vein distension
- Check laboratory findings (ECG, cardiac enzymes)
- Maintain intake
- Output chart
- Obtain daily weight
- Administer prescribed drugs like digitalis (risk for complications related to disease process)
Goal: to reduce risk of complications
Interventions
- Assess vital signs of patient
- Assess peripheral edema
- Check the laboratory findings (ECG, cardiac enzymes)
- Administer digitalis and digoxin if signs of heart failure appear
- Prepare for emergency pericardiocentesis