WHOOPING COUGH – PERTUSSIS – Definition, Pathology, Clinical Manifestations, Diagnosis, Treatment and Prevention
DEFINITION
The term pertussis, which means intensive cough, is an acute respiratory infection, seen more commonly in young children. The disease is also more serious in them. The term “whooping cough” is derived from the occurrence of progressive repetitive paroxysms of cough followed by inspiratory whoop. Natural pertussis infection and vaccination do not produce life-long immunity. The immunity wanes over a few decades. Since there is almost complete coverage of DPT vaccination in children, adolescents and adults may become susceptible to infection increasingly. It is therefore possible that adults develop pertussis infection.
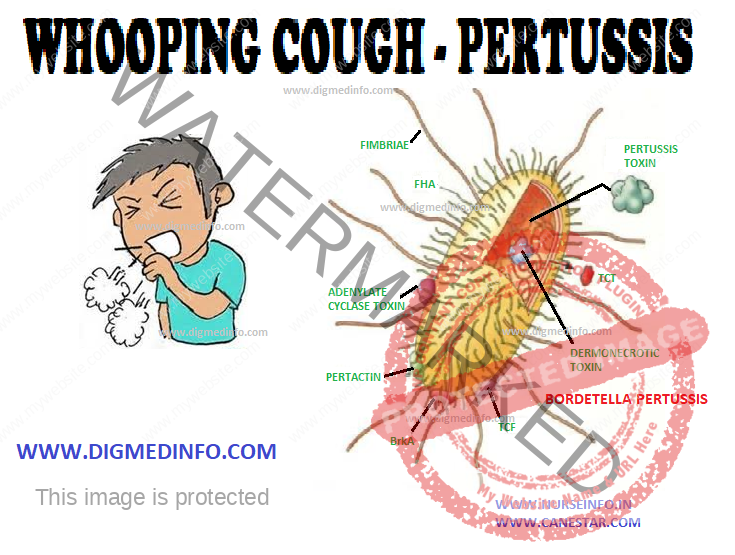
Pertussis is caused by Bordetella pertussis which is highly infective. Bordetella parapertussis and B. bronchiseptica are members of the same genus, rarely causing disease in man. Maximum incidence is seen in children below five years and the mortality is highest for children below 1 year of age. The organisms are spread by droplet infection and the route of entry is the respiratory tract.
The infectious period is the catarrhal prodrome and for three weeks after the onset of illness. Bordetella are small gram-negative coccobacilli, exclusively pathogenic to humans. The genome of B.pertussis has been sequenced.
Pathology
The mucosal lining of the respiratory tract shows inflammation. Peribronchial lymphoid hyperplasia occurs initially and this is followed by necrosis of the midzonal and basilar layers of the bronchial epithelium. This leads to the accumulation of tenacious mucus, atelectasis and eventually bronchiectasis.
Clinical Manifestations
The incubation period is usually 7-14 days but may be prolonged to 20 days. Three stages can be distinguished—catarrhal, paroxysmal and convalescent—each lasting up to 2 weeks so that the course of the disease extends to 6-8 weeks.
The catarrhal stage manifests with rhinorrhea, mild fever, and cough. During this stage, clinical recognition of the disease is difficult. This is the most infective stage.
In the paroxysmal stage cough starts, increases in severity, and becomes repetitive and explosive. Each paroxysm is followed by a whoop produced by a sudden massive inspiratory effort through a narrowed glottis. During the paroxysms of cough the infant develops facial congestion, distension of neck and scalp veins, lacrimation, cyanosis, and clouding of consciousness. The paroxysm ends with the onset of vomiting. The whoop may not be distinctly made out in younger infants, but they may become asphyxiated and develop anoxic convulsions. Physical examination may reveal periorbital edema. In the uncomplicated cases lung signs are usually absent. Pertussis occurring in adults causes prolonged cough. With increasing age the manifestations also become more severe.
Convalescence is marked by the decrease in frequency and severity of the paroxysms. Vomiting subsides and the patient’s appetite improves. At this stage the child is very susceptible to develop superinfections by other respiratory pathogens and this may lead to recurrence of the
paroxysms of cough. When this occurs it may last for several months.
Complications
Complications are common to develop
A. Respiratory:
Otitis media, especially in infants
Bronchitis
Bronchopneumonia
Atelectasis (segmental or lobar)
Interstitial or subcutaneous emphysema or pneumothorax due to rupture of alveoli
Bronchiectasis
Flare-up of tuberculosis
Sudden death of the infant may occur
B. Central nervous system:
Convulsions may occur due to anoxia, encephalopathy or rarely intracranial hemorrhage.
C. Gastrointestinal:
Severe vomiting with dehydration, tetany, ulceration of the frenum of the tongue (due to biting during a paroxysm), prolapse rectum, hernia.
D. Hemorrhages:
Epistaxis
Subconjunctival hemorrhage
Hemoptysis, hematemesis
E. Malnutrition:
Severe emaciation occurs in most of the affected children. In poor communities it is the starting point for marasmus and kwashiorkor.
Diagnosis
The disease has to be suspected clinically, particularly in an unimmunized child with known contact with the disease. Total leucocyte count is elevated to 20,000 to 50,000/cmm with absolute lymphocytosis. A leukemoid reaction may sometimes occur. Chest X-ray may show perihilar infiltrates or segmental collapse. Bacteriological diagnosis is established by culturing the organism obtained from nasopharyngeal swabs. Fluorescent antibody staining of pharyngeal specimens provides a rapid and specific diagnosis. PCR using nasopharyngeal aspirate reveals the organisms. In cases with duration above two weeks IgG antitoxic antibody can be demonstrated in serum.
Treatment
Supportive care is important to maintain nutrition, prevent aspiration into the respiratory tract and maintain the airway. The airway is cleared by suction of the exudates. Anoxic convulsions are managed by administration of oxygen and anti-convulsants. Small, frequent feeds are tolerated if given soon after a paroxysm of cough.
Intravenous fluids may be required if the child is dehydrated. In general, administration of antibiotics does not shorten the paroxysmal stage, once it is established. Erythromycin 50 mg/kg/day given for 5-7 days will reduce the period of communicability. It may even abort or prevent the progress of the disease if given in the catarrhal stage. Ampicillin, chloramphenicol and cotrimoxazole may also be used as alternative drugs. Azithromycin 250-500 mg po, od for 7-10 days is effective in controlling the infection if started early. Clarithromycin is a suitable alternative.
Antibodies are not transferred transplacentally in the case of whooping cough. In most patients, a single attack confers life-long immunity.
Prevention
Active immunization is achieved by the administration of the pertussis vaccine, usually given in combination with diphtheria and tetanus toxoids (DPT). The vaccine contains killed B. pertussis. The initial dose is given at 2 months, with 2 more doses at 4 week intervals. The first booster is given 1 year later and the next one at school entry.