VITAMIN – D – Biological Actions, Daily Requirements, Rickets, Clinical Features, Diagnosis, Treatment and Prevention
Vitamin D is required for normal metabolism of calcium and phosphorus and for bone formation. It enhances the absorption of these minerals from the gut, their mobilization from bone and the reabsorption of phosphorus by the kidney. Vitamin D1 is the essential precursor for 1-25 alpha dihydroxy vitamin D1 which is the steroid hormone required for the development of bone, growth in children, maintenance of bone mass in adults and also for the retardation of osteoporosis and prevention of fractures in the elderly.
The two different forms of vitamin D active in man are vitamin D (calciferol) obtained by ultraviolet irradiation of ergosterol (also called ergocalciferol or provitamin D2) which is of plant origin, and vitamin D3 (cholecalciferol) which is formed by activation of 7-dehydrocholesterol present in the epidermal cells of human skin as a provitamin D2. This activation is effected by the ultraviolet rays ranging in wavelength from 296 to 310 A obtained from sunlight naturally. Exposure to sunlight for 20-30 minutes daily ensures adequate supply of Vitamin D. Excessive exposure does not lead to overdose of the vitamin. Skin damaged by burns will not be capable of producing Vitamin D on exposure to sunlight.
Vitamin D2 is obtained from the diet and vitamin D3 is formed endogenously. On an average the endogenous source supplies about 80% and diet about 20% of the total requirement. Vitamin D2 and D3 which are identical in potency, differ only in the configuration of the side chain. Vitamin D3, though formed in the skin is also absorbed through the small intestine. Further metabolism of vitamin D2 and D3 is identical and these together are referred to as vitamin D.
Biological actions of vitamin D metabolites:
1. Increase the absorption of calcium and phosphate from the small intestine by promoting active transport.
2. Increase mobilization of calcium from bone by promoting osteoclastic activity.
3. Stimulation of reabsorption of calcium and phosphate at the renal tubules.
The overall result of all these processes is to increase serum calcium and phosphate. Deficiency of vitamin D results in impairment of mineralization of bone leading to nutritional rickets in children and osteomalacia in adults.
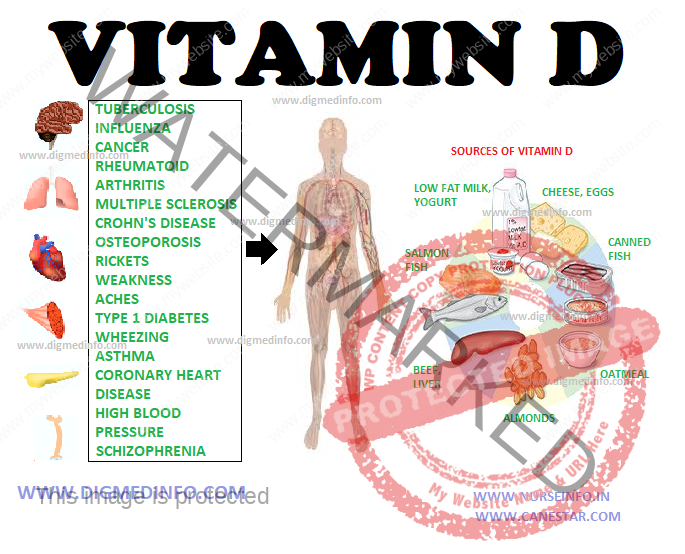
Dietary sources of vitamin D are milk, butter, cheese, egg yolk and fish liver oils. This vitamin is heat stable. One international unit (IU) is equivalent to 0.025 μg. The daily requirement varies depending on the age.
DAILY REQUIREMENTS
Infant and children – 400 IU
Age 19-50 years – 200 IU
51-70 years – 400 IU
71 and above years – 600 IU
RICKETS
Prevalence Rickets is prevalent in India, more so in the north than in the south. Premature babies are more vulnerable. The disease is more florid during winter months when exposure to sunlight is minimal. Prevalence is more among the poor and illiterate classes. Indians who have emigrated to affluent countries still show a higher prevalence of rickets. Osteomalacia is more common in multiparous women who have nursed their babies repeatedly. Rickets has been ranked among the most frequent childhood diseases affecting children in the developing world. There is evidence that dietary deficiency of calcium may also lead to rickets.
In rickets, the arrangement and normal regenerative processes of cartilage are abnormal. Subsequent calcification of the cartilaginous matrix and osteoid do not proceed normally. The osteoid and cartilage which remain uncalcified are deposited irregularly. These give rise to a wide irregular frayed zone of non-calcified cartilage and osteoid termed rachitic metaphysis. These in turn account for many of the skeletal deformities. In the subperiosteal region also, while resorption of cortical bone continues normally, new bone is not laid down, resulting in softening and rarefaction of the bone shaft. In vitamin D deficiency, since absorption of calcium and, phosphorus from the gut is defective, serum calcium and phosphorus levels fall. Lowered level of serum calcium stimulates the secretion of parathyroid hormone which in turn, leads to mobilization of calcium from the bone. Thus, the serum calcium is usually maintained normal for considerable periods, tetany developing only rarely. Since parathyroid hormone (PTH) decreases reabsorption of phosphorus by the renal tubule, the serum phosphorus falls. The serum alkaline-phosphatase is elevated due to increased osteoblastic activity.
CLINICAL FEATURES
Florid rickets manifests by the age of 1-2 years. Early manifestations These include irritability, flabbiness of muscles, prominence of abdomen and delay in the appearance of milestones, except speech. Skeletal manifestations These are the most characteristic features. They develop several months after the deficiency is established. The bones which have the maximum rate of growth at the time of onset of the deficiency show gross abnormalities.
In children below the age of 1 year the lesion is craniotabes, characterized by abnormal softening of the skull in the occipital region. In children aged 2 years or more epiphyses of the wrists and ankles are widened and costochondral junctions are enlarged and beaded. In advanced rickets, deformities of bones are aggravated because of muscular action, gravity and weight bearing.
Head
Craniotabes disappears by 1 year of age, but the excess of osteoid and non-calcified cartilage gives rise to frontal and parietal bossing giving the skull a ‘hot cross bun’ appearance. Due to softening of the skull bones the calvarium is asymmetric. The head may be larger in size and closure of the anterior fontanelle may be delayed. The teeth erupt late; show defective enamel, and are more susceptible to develop caries. Permanent teeth also show grooving, pitting and hypoplastic enamel.
Rib-cage
Costochondral junctions are thickened (rachitic rosary) and the sternum projects forwards (pigeon chest deformity). A horizontal groove (Harrison’s sulcus) develops along the diaphragmatic attachment due to
muscular pull of the diaphragm on the softened bone.
Spine
This shows kyphosis and scoliosis when the baby starts sitting and later lordosis in the erect posture.
Pelvis
In lordotic subjects the pelvis shows a corresponding deformity. The pelvis is small and deformed (triradiate pelvis), and in female subjects the obstruction caused to the pelvic outlet gives rise to dystocia during parturition.
Extremities
The femur, tibia and fibula bend producing deformities like knock knees, coxa vara, etc. The thickened epiphyseal ends may be more prominent. Deformities of upper limbs develop if rickets sets in when the infant is crawling. Long bones may develop green stick fractures and pseudofractures. The sum total of bony deformities of the spine, pelvis, and legs leads to rachitic dwarfism.
Other general manifestations include hepatosplenomegaly, tetany, laryngysmus stridulus, convulsions and frequent respiratory infections.
Diagnosis
Rickets should be suspected in any child showing deformities of skull, long bones and ribs and in those with apathy, flabbiness, delayed milestones of development, laryngysmus stridulus or convulsions.
The clinical diagnosis is supported by the history of inadequate vitamin D in the diet or chronic diarrhea interfering with absorption of vitamin D, and it is confirmed by radiological investigations and biochemical tests. X-ray findings in active rickets Routine skiagrams of the wrists give clues in diagnosis and are helpful for following the progress. The distal ends of radius and ulna appear concave (cupping), widened (flaring) and irregular (fraying). The distance between the distal ends of the ulna and the radius and the metacarpal bones is apparently increased since the uncalcified rachitic metaphyses is translucent to X-ray. Shafts of long bones show decreased density and prominent trabeculations. Subperiosteal osteoid may give a double contour to the shaft.
With treatment, the lesions tend to heal. A line of preparatory calcification (LPC) appears. This is separated from the distal end of the shaft by a zone of translucency caused by the uncalcified osteoid. As healing progresses, the osteoid becomes calcified and shaft apparently grows towards the LPC and unites with it.
Measurement of serum 25 hydroxy vitamin D gives a reliable indication of the adequacy of the nutritional status. Normal values are above 15 ng/mL. Values below 8 mg/mL indicate severe deficiency.
Biochemical changes
In florid cases the serum phosphorus is low (1.5-3.5 mg/dL) Serum calcium may usually be normal, but in advanced cases it is reduced especially in cases with tetany. Serum alkaline phosphatase is raised to 20-60 KA units/dL (Normal 5-15). With correction of the lesion alkaline phosphatase level falls and serum phosphorus level goes up. Normal serum vitamin D levels range from 35 ± 3.5 ng/mL (80 nmol/L) and 1,25 (OH)2 D is 35 ± 3 pg/mL.
In active rickets these levels are lowered.
Prognosis for growth and cosmetic recovery is excellent if the condition is recognized early and treated before deformities develop. Intercurrent infections make the prognosis worse. If treatment is started after the bony deformities are established and the epiphyses are ossified, the deformities tend to persist.
Treatment
Oral administration of vitamin D in doses of 1500-5000 IU daily brings about rapid improvement in the vast majority of cases. Radiological improvement will be demonstrable in 2-4 weeks. A single dose of 600,000 units is preferable for advanced cases. The dose may be given orally or as in intramuscular injection. An oily preparation is available for intramuscular injection which is effective for 3 months. Three to four injections are given at intervals of two weeks. Parenteral administration is mandatory in cases showing malabsorption. If there is no improvement even after two parenteral doses of vitamin D, the case is considered to be resistant to vitamin D.
After complete healing of the lesion vitamin D should be given in doses of 400 units daily for preventing recurrence. Children should be encouraged to get exposure to sun for 20-30 minutes daily. Early bone lesions will be corrected with simple medical treatment. If treatment is started late and deformities are permanent, orthopedic correction is indicated.
Vitamin D-resistant rickets
This may be acquired, as in chronic renal failure or inherited as in congenital enzyme defects.
In chronic renal failure conversion of 25-OH D3 into the active metabolite 1,25(OH)2D3 becomes defective due to the progressive deficiency of the enzyme in the renal tubules. Such patients develop features of rickets (renal rickets) forming part of renal bone diseases.
Inherited forms of rickets
Pseudo-vitamin D deficiency: Two types are known. Rickets develop early in life. Hypotonia, weakness, seizures and growth failure develop.
Vitamin D dependent rickets type I
This is an autosomal recessive trait in which the gene for expressing the renal enzyme 25 hydroxy vit D3 1-alpha hydroxylase is defective, and so this enzyme level is low or absent. Plasma levels of 25(OH)D3 are normal, but 1,25 (OH)2D3 are low. The gene is located on chromosomes X 12 q 13.3.
Vitamin D dependent rickets type II
Two forms exist. In one form, the gene for vitamin D receptor is mutated. Hypocalcemic rickets develops. In the second form, also known as X-linked hypophosphatemic vitamin D resistant rickets the phosphate regulating gene (PEX gene) with homology to endopeptidoses on the X chromosome is defective. All these forms respond to 1,25(OH)2 vitamin D.
HYPERVITAMINOSIS D
Prolonged administration of massive doses of vitamin D results in vitamin D intoxication. This causes hypercalcemia. Symptoms include nausea, vomiting, constipation, drowsiness, and signs of renal impairment. Metastatic calcification occurs in several tissues including
the kidneys, lungs, gastric mucosa and blood vessels. Renal function may deteriorate before other signs of toxicity are manifest. Subjects receiving high doses of vitamin D should have regular monitoring of serum calcium and if it is above 2.6 mmol/liter (10.5 mg/dL), the intake of the vitamin should be stopped.