TRIGEMINAL NEURALGIA (‘TIC DOULOUREUX’) – Etiology, Signs and Symptoms, Types and Management
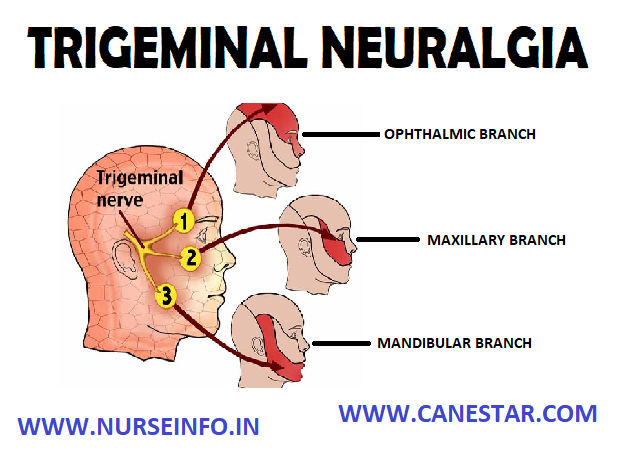
The trigeminal nerve (also called the fifth cranial nerve) is one of the main nerves of the face. It comes through the skull from the brain in front of the ear. It is called trigeminal as it splits into three main branches. Each branch divides into many smaller nerves. The nerves from the first branch go to scalp, forehead and around eye. The nerves from second branch go to the area around cheek. The nerves from the third branch go to the area around jaw. The branches of the trigeminal nerve take sensations of touch and pain to the brain from face, teeth and mouth. The trigeminal nerve also controls the muscles used in chewing and the production of saliva and tears.
In trigeminal neuralgia (TN) sudden pains that come from one or more branches of the trigeminal nerve. The pains are usually severe. The second and third branches are the most commonly affected. Therefore, the pain is usually around the cheek or jaw or both. The first branch is less commonly affected, so pain over forehead and around eye is less common. Trigeminal neuralgia usually affects one side of face.
ETIOLOGY
- Tumor
- Multiple sclerosis
- Abnormality of the base of the skull
SIGNS AND SYMPTOMS
Triggers of pain attacks include the following:
- Chewing, talking or smiling
- Drinking cold or hot fluids
- Touching, shaving, brushing teeth, blowing the nose
- Encountering cold air from an open automobile window
Pain localization is as follows:
- Patients can localize their pain precisely
- The pain commonly run along the line dividing either the mandibular and maxillary nerves or the mandibular and ophthalmic portions of the nerve
- The pain shoots from the corner of the mouth to the angle of the jaw
- Pain jolts from the upper lip or canine teeth to the eye and eyebrow
- Pain involves the ophthalmic branch of the facial nerve
The pain has the following qualities:
- Characteristically severe, paroxysmal and lancinating
- Commences with the sensation of electrical shocks in the affected areas
- Begins to fade within seconds, only to give way to a burning ache lasting seconds to minutes
- Pain fully abates between attacks, even when they are severe and frequent
- Attacks may provoke patients to grimace, wince, or make an aversive head movement, as if trying to escape the pain, thus producing an obvious movement, or tic, hence called ‘tic douloureux’.
TYPES OF ‘TIC DOULOUREUX’
Trigeminal neuralgia can be split into different categories depending on the type of pain. These are:
- Trigeminal neuralgia type 1 (TN1) is the classic form of trigeminal neuralgia. The piercing and stabbing pain only happens at certain times and is not constant. This type of neuralgia is known as idiopathic
- Trigeminal neuralgia type 2 (TN2) can be referred to as atypical trigeminal neuralgia. Pain is more constant and involves aching, throbbing and burning sensations
- Symptomatic trigeminal neuralgia (STN) is when pain results from an underlying cause, such as multiple sclerosis
MANAGEMENT
Medical Management
- The anticonvulsant carbamazepine is the first line treatment, second line medications include baclofen, lamotrigine, oxcarbazepine, phenytoin, gabapentin, pregabalin, and sodium valproate
- Low doses of some antidepressants such as amitriptyline are thought to be effective in treating neuropathic pain
- Duloxetine can also be used in some cases of neuropathic pain, and as it is also an antidepressant can be particularly helpful where neuropathic pain and depression are combined.
- Opiates such as morphine and oxycodone can be prescribed, and there is evidence of their effectiveness on neuropathic pain, especially if combined with gabapentin
- Gallium maltolate in a cream or ointment base has been reported to relieve refractory postherpetic trigeminal neuralgia
Deep Brain Stimulation
It involves delivering and electrical pulse to a part of the brain using a probe. A scanning technique (usually MRI or CT) is used to make sure the probe is in the right place
SURGICAL MANAGEMENT
An operation is an option if medication does not work or causes troublesome side-effects. Basically, surgery for trigeminal neuralgia falls into two categories:
- Decompression surgery: this means an operation to relieve the pressure on the trigeminal nerve. As trigeminal neuralgia are due to a blood vessel in the brain pressing on the trigeminal nerve as it leaves the skull. An operation can ease the pressure from the blood vessel (decompress the nerve) and therefore ease symptoms. This operation has the best chance of long-term relief of symptoms. However, it is a major operation involving a general anesthetic and brain surgery to get to the root of the nerve within the brain. Although usually successful, there is small risk of serious complications, such as a stroke or deafness, following this operation
- Ablative surgical treatments: ablative means to destroy. There are various procedures that can be used to destroy the root of the trigeminal nerve and thus ease symptoms. For example, one procedure is called stereotactic radiosurgery (gamma knife surgery). This uses radiation targeted at the trigeminal nerve root to destroy the nerve root. The advantage of these ablative procedures is that they can be done much more easily than decompression surgery as they do not involve formal brain surgery. So, there is much less risk of serious complications or death than there is with decompression surgery
- Balloon compression: it works by injuring the insulation on nerves that are involved with the sensation of light touch on the face. The procedure is performed in an operating room under general anesthesia. A tube called a cannula is inserted through the cheek and guided to where one branch of the trigeminal nerve passes through the base of the skull. A soft catheter with a balloon tip is threaded through the cannula and the balloon is inflated to squeeze part of the nerve against the hard edge of the brain covering and the skull. After about a minute the balloon is deflated and removed along with the catheter and cannula. Balloon compression is generally an outpatient procedure, although sometimes the patient may be kept in the hospital overnight. Pain relief usually lasts one to two years.
- Glycerol injection: it is also generally an outpatient procedure in which the individual is sedated with intravenous medication. A thin needle is passed through the cheek, next to the mouth and guided through the opening in the base of the skull where the third division of the trigeminal nerve (mandibular) exits. The needle is moved into the pocket of spinal fluid that surrounds the trigeminal nerve center. The procedure is performed with the person sitting up, since glycerol is heavier than spinal fluid and will then remain in the spinal fluid around the ganglion. The glycerol injection bathes the ganglion and damages the insulation of trigeminal nerve fibers. This form of rhizotomy is likely to result in recurrence of pain within a year to two years. However, the procedure can be repeated multiple times.
- Radiofrequency thermal lesioning (also known as ‘RF Ablation or ‘RF lesion’). It is most often performed on an outpatient basis. The individual is anesthetized and a hallow needle is passed through the cheek through the same opening at the base of the skull where the balloon compression and glycerol injections are performed. The individual is briefly awakened and a small electrical current is passed through the needle, causing tingling in the area of the nerve where the needle tips rests. When the needle is positioned so that the tingling occurs in the area of TN pain, the person is then sedated and the nerve area is gradually heated with an electrode, injuring the nerve fibers. The electrode and needle are then removed and the person is awakened. The procedure can be repeated until the desired amount of sensory loss is obtained; usually a blunting of sharp sensation, with preservation of touch.
- Stereotactic radiosurgery (gamma knife, cyber knife) uses computer imaging to direct highly focused beams of radiation at the site where the trigeminal nerve exits the brain stem. This causes the slow formation of a lesion on the nerve that disrupts the transmission of sensory signals to the brain.
- Microvascular decompression (MVD). It is the most invasive of all surgeries for trigeminal neuralgia, but also offers the lowest probability that pain will return. About half of individuals undergoing MVD for trigeminal neuralgia will experience recurrent pain within 12 or 15 years. This inpatient procedure, which is performed under general anesthesia, requires that a small opening be made through the mastoid bone behind the ear. While viewing the trigeminal nerve through a microscope or endoscope, the surgeon moves away the vessel (usually an artery) that is compressing the nerve and places a soft cushion between the nerve and the vessel. Unlike rhizotomies, the goal is not to produce numbness in the face after this surgery. Individuals generally recuperate for several days in the hospital following the procedure, and will generally need to recover for several weeks after the procedure
- Neurectomy (also called partial nerve section): which involves cutting part of the nerve, maybe performed near the entrance point of the nerve at the brain stem during an attempted microvascular decompression if no vessel is found to be pressing on the trigeminal nerve. Neurectomies are also performed by cutting superficial branches of the trigeminal nerve in the face. When done during microvascular decompression, a neurectomy will cause more long-lasting numbness in the area of the face that is supplied by the nerve or nerve branch that is cut. However, when the operation is performed in the face, the nerve may grow back and in time sensation may return. With neurectomy, there is risk of creating anesthesia dolorosa.
NURSING MANAGEMENT
Nursing Interventions
- Instruct the client to avoid factors that can trigger the attack and result in exhaustion and fatigue
- Avoid foods that are too cold or too hot
- Chew foods in the affected side
- Use cotton pads gently, wash face and for oral hygiene
- Provide teaching to clients who have sensory loss as a result of a treatment
- Inspection of the eye for foreign bodies, which the client will not be able to feel, should be done several times a day
- Warm normal saline irrigation of the affected eye two or three times a day is helpful in preventing corneal infection
- Dental checkup every 6 months is encouraged, since dental caries will not produce pain
- Explain to the client and his family the disease and its treatments