RESTRICTIVE LUNG DISEASES – Etiology, Pathophysiology, Signs and Symptoms, Diagnostic Evaluation and Management
Introduction
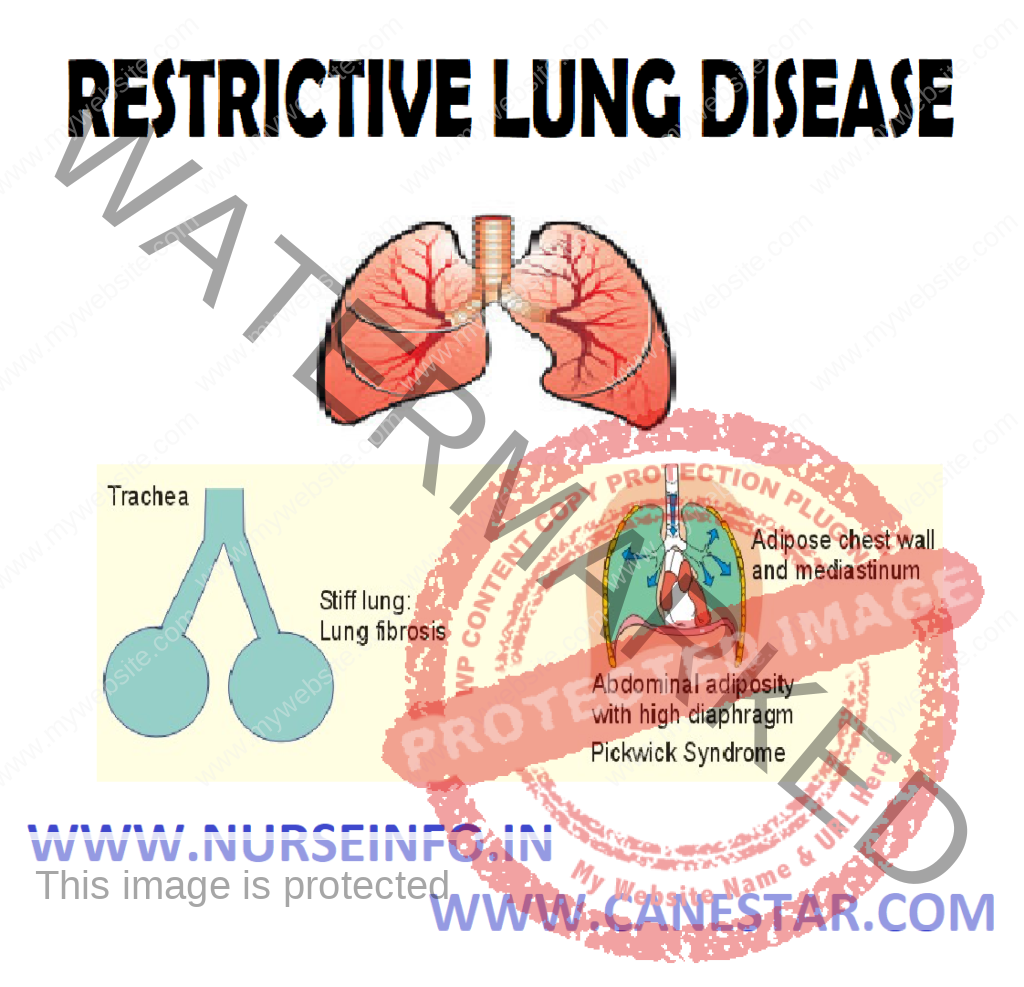
Restrictive lung diseases are characterized by reduced lung volume, either because of an alternation in lung parenchyma or because of a disease of the pleura, chest wall, or neuromuscular apparatus. In physiological terms, restrictive lung diseases are characterized by reduced total lung capacity (TLC), vital capacity, or resting lung volume. Accompanying characteristics are preserved airflow and normal airway resistance, which are measured as the functional residual capacity (FRC). If caused by parenchymal lung disease, restrictive lung disorders are accompanied by reduced gas transfer, which may be marked clinically by desaturation after exercise.
DEFINITION
- Restrictive lung disease is a chronic disorder that causes a decrease in the ability to expand the lung and sometimes makes it harder to get enough oxygen to meet the body’s needs. The most common restrictive lung diseases are:
Interstitial pulmonary fibrosis or interstitial lung disease (including sarcoidosis-granulomatous disorder)
- Restrictive lung diseases are characterized by reduced lung volume, either because of an alteration in lung parenchyma or because of a disease of the pleura, chest wall, or neuromuscular apparatus. In physiological terms, restrictive lung diseases are characterized by reduced total lung capacity (TLC), vital capacity, or resting lung volume
ETIOLOGY
Restrictive lung diseases may be due to specific causes which can be intrinsic to the parenchyma of the lung, or extrinsic to it
Intrinsic
- Radiation fibrosis, usually from the radiation given for cancer treatment
- Certain drugs such as bleomycin and methotrexate
- As a consequence of another disease such as rheumatoid arthritis
- Hypersensitivity pneumonitis due to an allergic reaction to inhaled particles
- Acute respiratory distress syndrome (ARDS), a severe lung condition occurring in response to a critical illness or injury
- Infant respiratory distress syndrome due to a deficiency of surfactant in the lungs of a baby born prematurely
Extrinsic
- Neuromuscular diseases, including Myasthenia gravis, and Guillain-Barre syndrome
- Nonmuscular diseases of the upper thorax, such as kyphosis and chest wall deformities
- Diseases restricting lower thoracic/abdominal volume (e.g. obesity, diaphragmatic hernia, or the presence of ascites)
- Pleural thickening
PATHOPHYSIOLOGY
In cases of Intrinsic Lung Disease
The physiological effects of diffuse parenchyma disorders —- reduce all lung volumes by the excessive elastic recoil of the lungs, in comparison to the outward recoil forces of the chest wall —- expiratory airflow is reduced in proportion to lung volume —- arterial hypoxemia in these disorders is primarily caused by ventilation-perfusion mismatch —- the diffusion of oxygen is impaired —- hypoxemia
In cases of Extrinsic Disorders
Disorders of the pleura and thoracic cage —- the total compliance by the respiratory system is reduced —- lung volumes are reduced as a result of atelectasis —- ventilation-perfusion mismatch and hypoxemia —- hypoxemia
SIGNS AND SYMPTOMS
Symptoms of restrictive lung disease include:
- Cough
- Shortness of breath
- Wheezing and chest pain
- Difficulty in inhaling and exhaling
- Wheezing and noisy breathing
- Coughing up blood
DIAGNOSTIC EVALUATION
Diagnostic testing for lung disease may include any of the following:
- Physical examination
In patients with intrinsic lung disorders may yield distinguishing physical findings. Those with chest wall disorders show obvious massive obesity and an abnormal configuration of the thoracic cage (e.g. kyphoscoliosis, spondylitis)
Cyanosis at rest is uncommon in persons with interstitial lung diseases, and this is usually a late manifestation of advanced disease
Digital clubbing is common in those with idiopathic pulmonary fibrosis
- Pulmonary function tests: spirometry provides an objective assessment of airflow obstruction and is important in staging asthma severity. It should be done on initial diagnosis of asthma, after treatment is started and symptoms have stabilized, and every 1 to 2 years afterward. Spirometry is used to measure the rate of airflow during maximal expiratory effort after maximal inhalation. It can be useful in differentiating between obstructive and restrictive lung disorders
- Chest X-ray: patient is made to stand in front of X-ray machine. Patient will be told to hold breath when the X-ray is taken. Two images are usually taken. You will need to stand against the machine, and then sideways. Air-space opacities suggest pulmonary hemorrhage
- CT scans: high-resolution CT scanning of the chest can be helpful, but the expense and high dose of radiation makes it inappropriate for every patient. Generally, complete scans only a few minutes. The newest multidetector scanners can image the entire body in less than 30 seconds
- Bronchoscopy: a bronchoscope is a device used to see the inside of the airways and lungs. The scope can be flexible or rigid. A flexible scope is almost always used. It is a tube less than one-half inch wide and about two feet long. In rare cases, a rigid bronchoscope is used. The scope is passed through mouth or nose through windpipe and into lungs. Going through the nose is a good way to look at the upper airways
- Pulse oximetry: pulse oximeters are noninvasive devices used to measure a patient’s blood-oxygen saturation level and pulse rate
- Lung biopsy: a lung biopsy is not always required to make a diagnosis in patients suggested to have interstitial lung diseases. A lung biopsy can provide information that may help lead to a specific diagnosis, help assess for disease activity, exclude neoplastic and infectious processes, establish a definitive diagnosis, and predict the prognosis
MANAGEMENT
Few medicines are available to treat most causes of restrictive lung disease. In cases of restrictive lung disease caused by ongoing inflammation, medicines that suppress the immune system may be used, including:
Corticosteroids (such as prednisone)
Corticosteroids are a first-line therapy but are associated with myriad adverse effects. Corticosteroids, the most commonly used drugs, halt or slow the progression of pulmonary parenchymal fibrosis with variable success. The optimal duration of therapy is not known, but treatment for 1-2 years is suggested
Cytotoxic Therapy
Immunosuppressive cytotoxic agents may be considered for patients who do not respond to steroids, experience adverse effects, or have contraindications to high-dose corticosteroid therapy. The failure of steroid therapy is defined as a fall in FVC or TLC by 10% a worsened radiographic appearance and a decreased gas exchange at rest or with exercise
- Azathioprine is less toxic than methotrexate or cyclophosphamide and may be preferred as a corticosteroid-sparing agent for disorders that are not life-threatening. A response to therapy may not occur for 3-6 months
- Because of potentially serious toxicities, cyclophosphamide is reserved for fulminant or severe inflammatory disorders refractory to alternate therapy
- Supplemental oxygen therapy may be necessary
- Mechanical breathing assistance may be helpful to some people with breathing difficulty from restrictive lung disease
- Inhalers
- Expectorants
- Antibiotics
- Chemotherapy
- In cases of obesity-related lung disease, weight loss and exercise can help reduce the resistance to breathing caused by excess fat
- Severe, end-stage restrictive lung disease (such as idiopathic pulmonary fibrosis) may be treated with lung transplantation