PERITONEAL DIALYSIS – Definition, Purpose, Indications, Advantage, Principles, Types, Advantages, Preparation of the Patient and Environment, Equipment, For Dressing Changes, Procedure and Complications (NURSING PROCEDURE)
DEFINITION
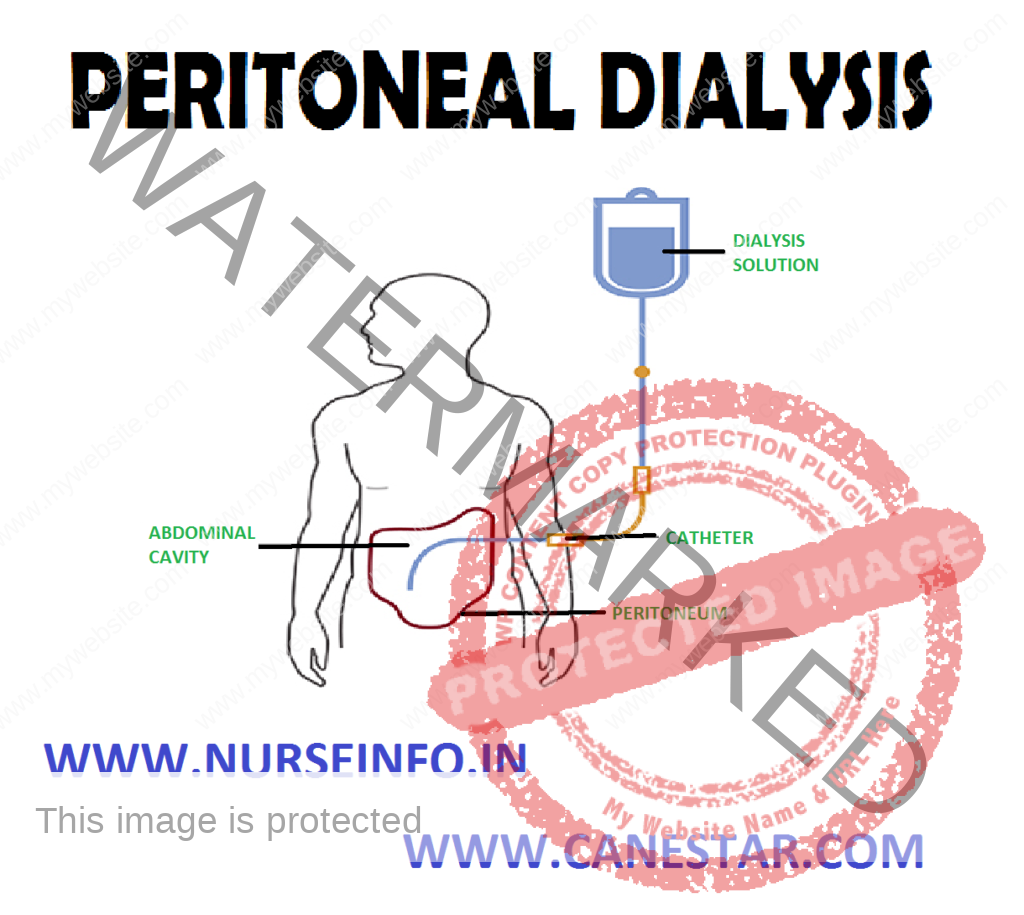
Peritoneal dialysis involves repeated cycles of instilling dialysis into the peritoneal cavity, allowing time for substance exchange, and then removing the dialysate
PURPOSE
- To remove the end products of protein metabolism such as urea and creatinine from the blood
- To maintain the safe concentration of seroelectrolytes
- To correct acidosis and replenish the bloods bicarbonate buffer system
- To remove excess fluid from the blood
INDICATIONS
Peritoneal dialysis is indicated for patients with:
- Chronic renal failure
- Cardiovascular instability
- Vascular access problems that prevent hemodialysis, fluid overload or electrolyte imbalance
- It has been used for overdose of drugs and toxins
ADVANTAGES
- One of the primary advantages of peritoneal dialysis is its relative indication which allows it to be used in community healthcare facilities without all the sophisticated equipment needed for dialysis
- It can be easily managed at home and often provide the client more independent and mobility and hemodialysis
PRINCIPLES OF PERITONEAL DIALYSIS
Diffusion: in diffusion, particles move through a semi-permeable membrane from an area of high-solute concentration to an area of low solute concentration
In peritoneal dialysis, the water-based dialysate being infused contains glucose, sodium chloride, calcium, magnesium, acetate or lactate and no waste products
Therefore, the waste products and excess electrolytes in the blood cross in the semi-permeable peritoneal membrane into the dialysate
Osmosis: in osmosis the fluids move through a semi-permeable membrane from an area of low solute concentration to an area of high solute concentration
In peritoneal dialysis dextrose is added to the dialysate to give it a higher solute concentration, then the blood, creating a high osmotic gradient
Water migrates from the blood through the membrane at the beginning of each infusion which the osmotic gradient is highest
TYPES OF PERITONEAL DIALYSIS
Continuous Abdominoperitoneal Dialysis (CAPD)
- The dialysate is instilled into the abdomen and left in the place for 4-8 hours
- The empty dialysate back is folded up and carried in a pouch or packet, until it is time to drain the dialysate
- The bag is later unfolded and placed lower than the insertion site, so the fluid drains by gravity flow
- When full the bag is changed, the new dialysate is instilled into the abdomen as the process continues
ADVANTAGES
- Because there is no need for electricity, water. The client can go about almost any desired activity during dialysis
- Because the continuous exchange process closely resembles normal renal function, the body more easily maintains homeostasis
Continuous Cycle Peritoneal Dialysis (CCPD)
- CCPD is similar to CAPD in that it is a continuous dialysis processes but different in that it requires a peritoneal cycling machine
- In this procedure, usually three cycles are done at night and one cycle within an 8 hours well done in the morning
Advantage
The advantage of this procedure is that the peritoneal catheter is opened only for the on and off procedures, which reduces the risk of infection
Intermittent Peritoneal Dialysis (IPD)
- IPD is not a continuous dialysis procedure like CAPD and CCPD
- Dialysis is performed 10-14 hours 3-4 times a week with use of same peritoneal cycling machine as in CCPD. Hospitalized patients may be dialysate up to 24-48 hours at a time if they are catabolic and require additional dialysis time
Contraindications
- Hypercatabolism, in which the peritoneal dialysis is unable to adequate the clear uremic toxins and poor condition of the peritoneal membrane due to adhesions and scaring
- Certain other conditions may be relative contra-indications to peritoneal dialysis. These include obesity, history of rupture diverticula, abdominal diseases, respiratory disease, recurrent episodes, abdominal malignancies, severe vascular diseases and extensive abdominal surgery with drains in tubes that may increase risk of infections
PREPARATION OF THE PATIENT AND ENVIRONMENT
- Bring all equipment into patient’s bedside
- Make sure the dialysis stat is at body temperature
- Explain the procedure to the patient. Assist and record vital signs, weight and abdominal girth to establish baseline levels
- Review recent laboratory values (blood urea, nitrogen, serum creatinine, sodium, potassium do complete blood counts). Identify the patient’s hepatitis b virus and human immunodeficiency virus if known
- Have the patient try to urinate
- Place the patient in the supine position, and have him put on one of the sterile face mask
- Informed concern must be obtained
- Baseline weight vital signs and blood chemistry provide important data for late comparison
- Mild sedation may be provided
EQUIPMENT
Catheter Placement and Dialysis
- Warmer heating pad or water bath
- At least three face masks
- Dialysis administration
- Two pairs of sterile gloves
- Vial of 1%
- Povidone-iodine pads
- Fenestrated sterile drape
- The 3 ml syringe with 25 G 1” needle
- Peritoneal stylet
- Sutures or hypoallergic tape
- Precut drain dressings
- Protective cap for catheter
- Precut drain dressings
- Protective cap for catheter
FOR DRESSING CHANGES
- One pair of sterile gloves
- Ten sterile cotton tipped applicators or sterile 2” multiply 2” gauze pads
- Povidone-iodine ointment
- Two sterile 4” multiply 4” gauze pads
PROCEDURE
- Wash your hands
- Inspect the warmed dialysate which should appear clear and colorless
- Put on a sterile face mask. Prepare to add any prescribed medication to the dialysate
- Prepare the dialysis administration set
- Close the clamps on all lines. Place the drainage bag below the patient to facilitate gravity drainage
- At this point the doctor puts on a mask and a pair of sterile gloves. He cleans the patient’s abdomen with povidone solution and drapes it with a sterile drape
- Wipe the stopper of the lidocaine vial with povidone iodine and allow it to dry. Invert the vial and hand it to the doctor so he can withdraw the lidocaine, using the 3ml syringe with the 25 C 1” needle
- The doctor anesthetizes a small area of the patient’s abdomen below the umbilicus. He then makes a small incision with the scalpel, inserts the catheter and sutures or tapes the catheter in place
- If the catheter is already in place, clean the site with povidone-iodine solution in a circular outward motion, according to your facility’s policy before each dialysis treatment
- Connect the catheter to the administration set, using aseptic technique to prevent contamination of the catheter and the solution, which could cause peritonitis
- Open the drain dressing and the 4” multiply 4” gauze pad pack ages. Put on the other pair of sterile gloves. Apply the precut drain dressings around the catheter. Cover them with the gauze pads and tape them securely
- Unclamp the lines to the patient. Rapidly instill 500 ml of dialysate into the peritoneal cavity to test the catheter’s patency
- Clamp the lines to the patient. Immediately unclamp the lines to the drainage bag to allow fluid to drain into the bag. Outflow should be risk
- Having established the catheter’s patency, clamp the lines to the drainage bag and unclamp the lines to the patient to infuse the prescribed volume of solution over a period of 5-10 minutes. As soon as the dialysate container empties, clamp the lines to the patient immediately to prevent air from preventing entering the tubing
COMPLICATIONS
- Peritonitis, the most common complication, usually follows contamination of the dialysate, but it may develop if solution leaks from the catheter exit site and flows back into the catheter tract. Respiratory distress may result when dialysate in the peritoneal cavity increases pressure on the diaphragm, which decreases lung expansion
- Protein depletion may result from the diffusion of protein in the blood into the dialysate solution through the peritoneal membrane. As much as ½ (14 g) of protein may be lost daily – more in patients with peritonitis
- Constipation is a major cause of inflow – outflow problems, therefore to ensure regular bowel movements, give a laxative or stool softener as needed
- Excessive fluid loss from the use of 4.25% solution may cause hypovolemia, hypotension, and shock. Excessive fluid retention may lead to blood volume expansion, hypertension, peripheral edema and even pulmonary edema and congestive heart failure
- Other possible complications include electrolyte imbalance and hyperglycemia, which can be identified by frequent blood tests