OSTEOMALACIA – Definition, Etiology, Clinical Features and Treatment
Definition
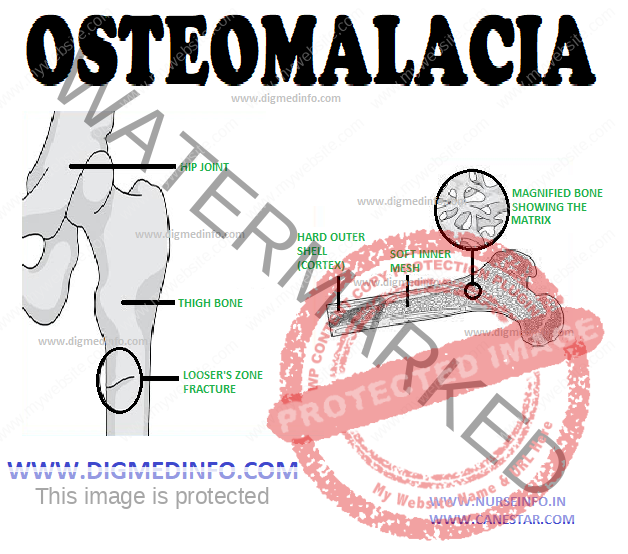
Osteomalacia denotes those disorders where mineralization of newly formed bone matrix (osteoid) is defective.
Etiology
Osteomalacia may be of two different types:
1. Nutritional inadequacy of vitamin D, calcium or both.
2. Vitamin D-resistant osteomalacia. The latter occurs in the following conditions.
a. In renal tubular defects which produce hypophosphatemia
and chronic metabolic acidosis.
b. Chronic administration of diphenylhydantoin which leads to excessive metabolism of vitamin D.
c. Osteoporosis.
d. After parathyroidectomy for osteitis fibrosa or hyperthyroidism in which rapid formation of new bone outstrips bone resorption.
Clinical features
Osteomalacia presents with vague pain which starts as aches and pains insidiously, in the lumbar spine and thighs and spreading later to the arms and ribs.
The pain is frequently felt over the bones themselves, and
not at the joints. The pain is usually symmetrical and nonradiating
and is accompanied by tenderness of involved bones. Proximal muscles are weak and there is difficulty in climbing up stairs and getting up from squatting position. Occasionally, localized acute bone pain develops rapidly. These sites correspond to the development of pseudofractures. Classical radicular pain may develop due to compression fracture of the vertebra.
Physical signs include deformities, which may be missed if not specifically looked for. The usual deformities are triradiate pelvis and spinal kyphosis (due to action of gravity). Pathologic fractures due to weight bearing and avulsion of tendinous attachments may develop. Biochemical features resemble those of rickets.
Characteristic radiological features are the appearance of “pseudofractures” (Milkman’s lines and Loser’s zones). These are linear zones of decalcification which tend to be symmetrical and extend perpendicular to the cortex. The common sites are the pubic rami, ischium, the neck of the femur, the outer edge of the scapula, ribs and vertebrae. Occasionally, Loser’s zones may extend right across a long bone simulating complete fractures. They are called pseudofractures because the gap is bridged by uncalcified osteoid tissue. They do not reveal any discontinuity of bone clinically. The pseudofractures are caused by the decalcification along the course of the major arteries entering the bones especially in areas of muscular attachment, namely the adductor insertion in the pubic ramus and attachment of gluteal muscles to the trochanters of the femur.
Vertebral bodies show compression and widening of intervertebral spaces to produce biconcave or “cod-fish” vertebrae.
However, in patients who develop osteomalacia secondary to renal tubular disorders or chronic renal failure, there is marked cortical thickening and increased density of trabeculae in spongy bone. The reason for this hyperosteosis is not clear. Despite the radiological appearances the bone is abnormally brittle and prone to develop fractures.
Treatment
Nutritional osteomalacia responds well to daily administration of 2000-4000 IU of vitamin D (0.05-0.1 mg) for 6-12 weeks followed by maintenance doses of 400-600 IU daily.
Dietary supplementation of calcium in the form of milk 500 mL per day hastens recovery. Medicinal calcium in the form of calcium gluconate, lactate or carbonate can be given as tablets or suspensions orally in doses of 250 to 500 mg daily. Supplementation has to be continued as long as the diet is deficient in calcium. Adequate supplements of calcium are provided in the form of milk 500-750 mL per day or calcium lactate tablets 1 g along with food.