ORGANOPHOSPHORUS COMPOUNDS – General Features, Clinical Features, Diagnosis and Treatment
General Features
These are the most widely used toxic agents for suicidal poisoning. Accidental poisoning occurs in workmen engaged in spraying operations. Contamination of food materials during storage or transportation has led to dramatic outbreaks of food poisoning. A dose of 40-100 mg proves fatal.
The commonly available products are methyl parathion (Folidol, Paramar, Metacid, Paramet), malathion (Malathion, Cythion) and phalone (Zolone, Sumithion, Faithion, Timidan, Ektakin). Organophosphorus compounds irreversibly phosphorylate acetyle cholinesterase (AChE) leading to the accumulation of acetyl choline at the cholinergic nerve endings such as autonomic ganglia, parasympathetic nerve endings and motor end plates.
CLINICAL FEATURES
Symptoms start within 15-30 minutes after ingestion of the toxin. Consumption on an empty stomach and along with alcohol favours rapid absorption.
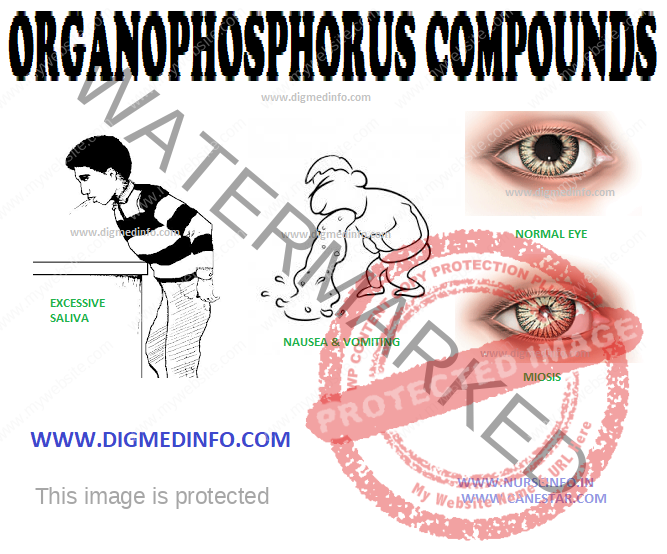
Gastrointestinal or neurological symptoms may predominate. Nausea, vomiting, diarrhea, involuntary defecation, blurring of vision, miosis, excessive sweating, lacrimation, salivation, and pulmonary edema constitute the muscarinic effects. Effects on central nervous system include drowsiness, coma, convulsions, and respiratory depression. Stimulation of pre-ganglionic fibres leads to sympathetic overaction and later paralysis, muscle twitching, fasciculation, weakness, and flaccid paralysis (nicotinic effects).
Diagnosis
In almost all cases, history, circumstances and the smell of the poison help to confirm the diagnosis. The chemical compound can be identified by examination of gastric contains and blood.
Diagnosis is clinical, supported by evidence of consumption of the poison. Estimation of serum levels of pseudocholinesterase is helpful. Normal level of pseudocholine esterase in serum is 1750-3500 μU/mL. Serum levels of the enzyme correlate inversely with the severity.
TREATMENT
The general measures for oral poisons should be instituted without delay.
Atropine
Atropine is the pharmacological antidote, and it is the sheet anchor of treatment since it antagonizes the peripheral effects of acetylcholine. It is freely available in all hospitals and cheap. This drug prevents pulmonary edema and excessive secretions. The dose requirement varies widely. In general, large doses have to be used. The ideal way to administer the drug is through an intravenous 5% glucose drip. A dose of 2 mg is given initially and 1 mg or more is repeated every 10 minutes (or even at shorter intervals) till the pupils are dilated to normal size and pulmonary edema and bronchorrhea is cleared. In many cases heroic doses, often several hundred ampoules of atropine may be required within a few hours to tide over the crises. The patient has to be observed very closely to prevent deterioration and death.
Maintenance dose is continued to keep the pupils in mid-dilation. It is usually possible to withdraw atropine after 24-48 hours but in some cases it may have to be continued for up to 5 days. Release of the toxin from lipid tissues after an interval of 2-3 days may result in return of symptoms and death after a period of apparent recovery. Hence, all patients have to be closely watched for at least 7 days after onset of the symptoms. In such cases, repetition of massive doses of atropine and supportive measures are to be undertaken.
Pralidoxime Hydrochloride
Pralidoxime hydrochloride is the specific antidote. It is given IV in a dose of 1-2 g initially and repeated 2-3 hrs later. It is available as 500 mg in 20 mL vials. Pralidoxime hydrochloride reactivates cholinesterase enzyme at the neuromuscular junctions by removing the phosphate group bound to the cholinesterase. It also binds to free organophosphate. The toxic effects of pralidoxime include tachycardia, cardiac arrhythmias, tachypnea, hypertension and relaxation of sphincters. The commercial preparation is 2 pyridine aldoxime (“aldopam”). Pralidoxime methane sulphate is also available.
In addition to pralidoxime, atropine has to be continued for symptomatic therapy in the required doses till the enzyme levels reach normal.
A high dose regimen of pralidoxime consisting of a continuous infusion of 1g/h for 48 hours after a 2 g loading dose reduces morbidity and mortality in moderally severe cases of acute organophosphorus pesticide toxicity. This reduces the need for atropine, as well as duration of ventilatory support.
Complications
Fatal bronchopneumonia may develop during convalescence. The neurological complications may take the form of intermediate syndrome occurring within 1-4 days of poisoning, characterized by bulbar, nuchal and proximal muscle weakness including respiratory paralysis or a distal sensorimotor polyneuropathy occurring 2-3 weeks later. The onset of intermediate syndrome usually coincides with the time of atropine withdrawal. Therefore oximes and atropine should be withdrawn carefully and gradually.
Prevention and first aid
Accidental poisoning can be prevented by taking adequate precautions detailed on the commercial packing. Persons spraying insecticides should wear protective clothing and masks, and wash their bodies with soap and water thoroughly after the work, and before taking food or drink. Immediate first aid after accidental poisoning includes induction of emesis and removal of contaminated clothing and washing the body thoroughly with soap and water. The subject should be transported to a hospital without delay.