LEUKEMIA – Etiology and Pathophysiology, Risk Factors, Clinical Manifestations, Classification, treatment and Management
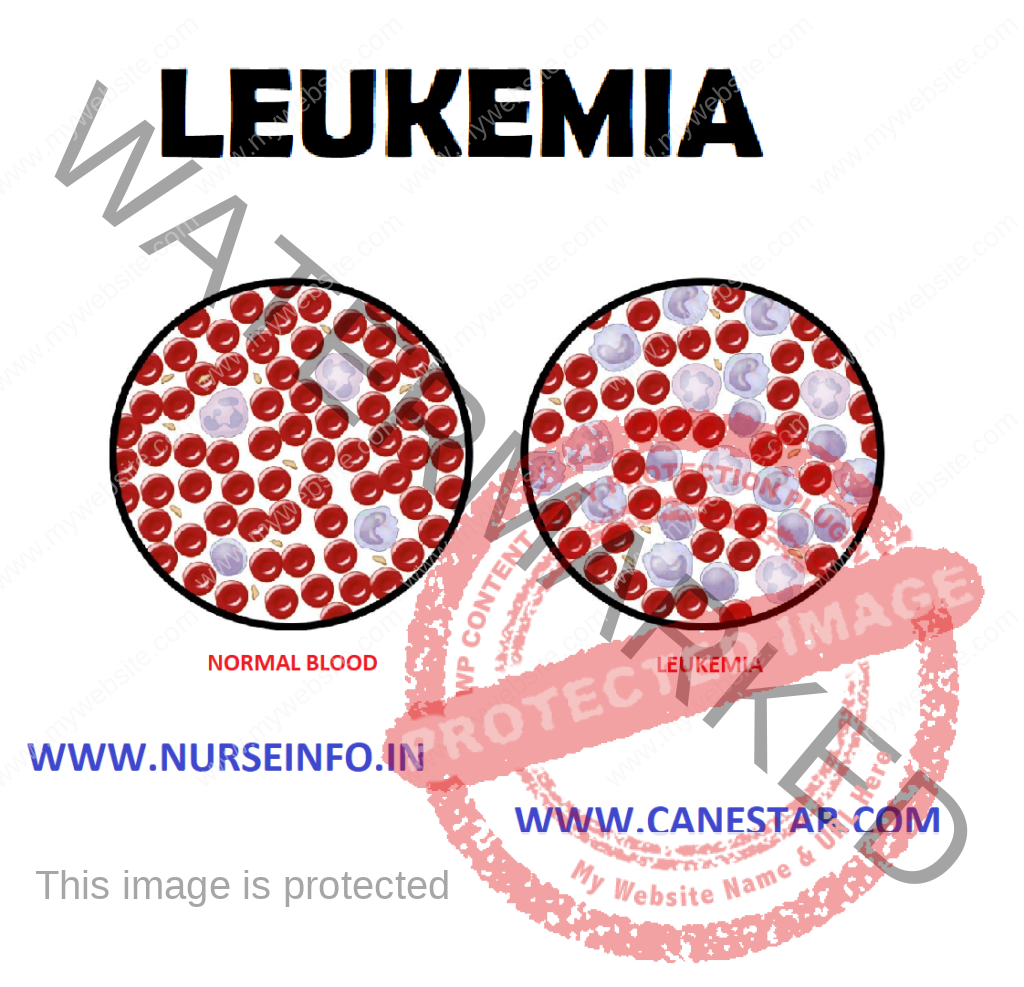
Leukemia is a type of cancer of the blood or bone marrow characterized by an abnormal increase of immature white blood cells called ‘blasts’. In turn, it is part of the even broader group of diseases affecting the blood, bone marrow, and lymphoid system, which are also known as hematological neoplasms.
ETIOLOGY AND PATHOPHYSIOLOGY
There are different causes:
The following are either known causes, or strongly suspected causes:
- Artificial ionizing radiation
- Viruses-HTLV-1 (Human T-lymphotropic virus) and HIV (Human immunodeficiency virus)
- Benzene and some petrochemicals
- Alkylating chemotherapy agents used in previous cancers
- Meternal fetal transmission
- Hair dyes
- Genetic predisposition
- Down syndrome – people with Down syndrome have a significantly higher risk of developing leukemia, compared to people who do not have Down syndrome.
RISK FACTORS
- Gender: men are more likely to develop CML, CLL and AML than women
- Age: the risk of most leukemias, with the exception of ALL, typically increases with age
- Genetics: family history: most leukemias have no familial link. However, first degree relatives of CLL patients, or having an identical twin who has or had AML or ALL, may at an increased risk for developing the disease
- Lifestyle: smoking: although smoking may not be a direct cause of leukemia, smoking cigarettes does increase the risk of developing AML
- Exposures: exposure to high levels of radiation: exposure to high-energy radiation (e.g. atomic bomb explosions) and intense exposure to low-energy radiation from electromagnetic fields (e.g. power lines)
- Chemical exposure: long-term exposure to certain pesticides or industrial chemicals like benzene is considered to be a risk for leukemia
- Previous Treatment: previous cancer treatment: certain types of chemotherapy and radiation therapy for other cancers are considered leukemia risk factors
CLINICAL MANIFESTATION
- Fever and night sweats
- Headache
- Bruising or bleeding
- Bone or joint pain
- A swollen or painful abdomen from an enlarged spleen
- Swollen lymph nodes in the armpit, neck or groin
- Getting a lot of infections
- Feeling very tired or weak
- Losing weight and not feeling hungry
- Fatigue
- Night sweat, lethargy
- Fever
CLASSIFICATION
- ALL (Acute lymphatic leukemia)
- ALM (Acute myelogenous leukemia)
- CLL (Chronic lymphocytic leukemia)
- CML (Chronic myelogenous leukemia)
ALL (Acute Lymphatic Leukemia)
It is a type of leukemia that, all types of leukemia starts from white blood cells in the bone marrow, the soft inner part of bones. It develops from cells called lymphocytes, type of WBCs central to immune system, an immature type of lymphocyte
CLINICAL MANIFESTIONS
- Fever
- Pallor
- Bleeding
- Anorexia
- Fatigue
- Weakness
- Bone, joint and abdominal pain
- Increase intracranial pressure
Acute Myelogenous Leukemia (AML)
It is fast growing cancer of the blood and bone marrow where the bone marrow makes many cancerous cells called leukemic blasts, normally blasts develop into WBCs that fight infection, but in AML, leukemic blasts do not develop properly and cannot fight infection. In this there is proliferation of immature myeloid cells
TREATMENT
- Use of cytarabine, 6-thioguanine and doxorubicin
- The same care of client as ALL, plus give adequate amounts of fluids (2000 to 3000 ml per day)
- Instruct client about medication, effects, side effects and nursing measures
Chronic Lymphocytic Leukemia (CLL)
It is a type of cancer of the blood or bone marrow, normally bone makes blood stem cells over the time
PATHOPHYSIOLOGY
- It is characterized by proliferation of small, abnormal, mature B lymphocytes, often leading to decreased synthesis of immunoglobulin and depressed antibody response.
- The number of mature lymphocytes in peripheral blood smear and bone marrow are greatly increased
CLINICAL MANIFESTATION
- Usually there is no symptoms
- Chronic fatigue, weakness, anorexia, splenomegaly, lymphadenopathy, hepatomegaly
- Skin lesions
- Anemia
- Thrombocytopenia
- The WBC count is elevated to a level between 20,000 to 100,000
- Increase blood viscosity and clotting episode
Chronic Myelogenous Leukemia (CML)
It is a type of cancer that starts in certain blood forming cells of the bone marrow. And in this bone marrow produces too many white cells. It affects the blood and bone marrow
- Occurs between 25-60 years of age. Peak 45 years and it caused by benzene exposure and high doses of radiation
CLINICAL MANIFESTATION
The classic symptoms of chronic types of leukemia include:
- Fatigue, weakness, fever, sterna tenderness
- Weight loss, joint and bone pain
- Massive splenomegaly and increase in sweating
- The accelerated phase of disease (blostic phase) is characterized by increasing number of granulocytes in the peripheral blood
- There is a corresponding anemia and thrombocytopenia
DIAGNOSTIC EVALUATION
- History: ask the patient for the presence of signs and symptoms. Assess the patient for the exposure of any risk factors or any history of risk factors
- Physical examination: during the physical examination, assess patient for sign and symptoms
- Assess patient for enlarged lymph nodes, areas of bruising, or any sign of infection
- Assess the vital signs of patient
- Complete blood count: in complete blood count, it measures the number of red blood cells, white blood cells and platelets. Most of patient with ALL has too many immature white cells. Low RBCs count, Hb, low platelet count, low to high WBC count
TREATMENT
Chemotherapeutic agent, it involve three phases
- Induction: during the induction phase the client receives an intensive course of chemotherapy designed to induce a complete remission of the disease. Once the remission is achieved the consolidation phase begins. Using vincristine and prednisone
- Consolidation: use modified course of intensive therapy to eradicate any remaining disease
- Maintenance: during the maintenance phase small doses of different combinations of chemotherapeutic agents are given every 3 to 4 weeks. It allows the client to live a normal life as possible
Other Management
- Eat diet that contains high in protein, fibers and fluids
- Avoid infection (handwashing, avoid crowds), injury
- Take measure to decrease nausea and to promote appetite, smoking and spicy and hot foods
- Maintain oral hygiene
Symptom Control
- Chemotherapy with chlorambucil, cyclophosphamide and prednisone to decrease lymphadenopathy and splenomegaly
- Splenic irradiation or splenectomy for painful splenomegaly or platelet sequestration hemolytic anemia
- Irradiation of painful enlarged lymph nodes
Supportive Care
- Transfusion therapy to replace platelets and RBCs
- IV immunoglobulins or gamma globulin to treat hypogamma globulinemia
Chronic Phase
- Palliative treatment, controlling symptoms, includes chemotherapy, irradiation, splenectomy
- Potentially curative treatment is offered by allogeneic (related to cumulated donor) BMT
Accelerated Phase or Blast Crisis
Attempts to restore chronic phase through use of high dose chemotherapy, leukophoresis
Nursing Intervention
- Taking measures to prevent infection
- Promoting safety
- Providing oral hygiene
- Preventing fatigue
- Promoting effective coping
- Client and family education
Nursing Assessment
History
- Ask patient for their family history, past medical history
- Ask for the presence of exposure to any risk factors and etiology factors
- Ask client for the presence of sign and symptoms
Physical Examination
- Asses for swollen lymph nodes, spleen or liver
- Assess the client vital signs. Check client for presence of fever
- Assess patient for the enlarged lymph nodes, sign of infection, and any signs of bruising or bleeding from any sites
Blood Tests
The lab does a complete blood count to check the number of white blood cells, red blood cells, and platelets. Leukemia causes a very high level of white blood cells. It may also cause low levels of platelets and hemoglobin, which is found inside red blood cells
Bone Marrow Aspiration
The doctor uses a thick, hollow needle to remove samples of bone marrow. The sample is taken from the back of the pelvic (hip) bone and with help of needle small amount of liquid bone marrow is sucked
Bone Marrow Biopsy
It is usually done just after the aspiration. The doctor uses a very thick, hollow needle to remove a small piece of bone and bone marrow
Nursing Diagnosis
- Impaired tissue integrity related to high dose radiation therapy
- Risk for infection to decreased neutrophils, altered response to microbial invasion, and presence of environmental pathogens
- Impaired oral mucous membrane related to low platelet count and effects of pathologic conditions and treatment as evidenced by oral bleeding
- Risk for injury related to low platelet counts and treatment
- Acute pain related to tumor growth, infection or adverse effects of chemotherapy
- Activity intolerance related to anemia and adverse effect of chemotherapy
Nursing Interventions
Maintain Tissue Integrity
- Avoid rubbing powders, deodorants, lotions or ointments (unless prescribed) or application of heat and cold to treated areas
- Encourage the patient to keep the treated area clean and dry
- Advise the patient to bath the area gently with tepid water and mild soap
- Encourage the patient to wear loose fitting cloths
- Advisee the patient to protect skin from over and direct exposure to sun light, chlorine and temperature extremes
Prevent from Infection
- Inspect the patient for the sign and symptoms of infection, e.g. redness, etc
- Maintain asepsis for patient at risk
- Instruct the patient to take antibiotics as prescribed by doctor to prevent microbial resistance
- Teach the patient and family how to avoid infections, e.g. about personal hygiene technique of handwashing, oral care, skin hygiene etc
- Educate the patient to report if there is any presence of signs of infection to the doctor immediately
- Monitor granulocyte count and WBC count to identify the presence of infection
- Screen all visitors for communicable diseases
Free the Mucosa from Bleeding
- Monitor lips, tongue, mucous membrane, and gums for moisture, color, texture, presence of infection
- Assist the patient to select soft, bland and nonacidic foods to decrease irritation of oral mucosa
- Advise the patient to use soft toothbrush for removal of dental debris
- Instruct the patient to perform oral hygiene after eating and as often as needed to avoid breakdown of oral mucosa
- Advise the patient to avoid the use of lemon glycerin swabs to prevent excessive drying of the mucosa
Health Education
- Teach the patient about the risk of infection and how to prevent from infection
- Educate the patient how to take medications, as ordered and instruct to avoid adverse effect and progress of diseases
- Provide patient and family member information about resources in the community, such as leukemia and lymphoma
- Educate the patient to maintain proper personal hygiene
- Teach the patient to avoid aspirin and NSAIDs which may interfere with platelet function
COMPLICATIONS
- Infections
- Blood problems
- Impaired body function
- Other cancers
- Leads to death
- Infections: leukemia causes abnormalities in the white blood cells. While healthy white blood cells protect the body against infections and disease, defective cells lose this ability. Without the protective properties of the white blood cells, people with leukemia become more susceptible to infections, which are the most common leukemia complications involved with the disease
- Blood Problems: people with leukemia may experience complications related to the blood. In some people, leukemia may lead to excess bleeding or bruising. Both may occur when leukemia causes a shortage in the number of platelets in the body. Other people experience an increase in the number of platelets, which can lead to clogging or excessive blood clotting
- Impaired Body Functions: when one part of the body begins to malfunction, it can lead to complications in other parts of the body. In the case of leukemia, the disease may adversely affect the spleen, kidneys, and renal areas. In a healthy body, the spleen stores excess blood cells. When levels increase due to leukemia, the spleen may attempt to store more than it can hold, which can cause an enlarged spleen
- Death: like most diseases without a care, possible death is another complication of leukemia