INTESTINAL OBSTRUCTION – Etiology, Risk Factors, Types, Signs and Symptoms, Pathophysiology, Diagnostic Evaluations and Management
Intestinal obstruction is an interruption in the normal flow of intestinal contents along the intestinal tract. The obstruction may occur in small intestine or colon and can be partial or complete, may be mechanical or may be paralytic, may or may not comprise of the vascular supply.
Intestinal obstruction exists when there is blockage, mechanical or functional, that prevents the normal flow of the intestinal contents through the intestinal tracts. It can occur at any level distal to the small intestine or large intestine and is a medical emergency
ETIOLOGY
- Obstructions of the small intestine may be caused by narrowing of the intestinal lumen as a result of inflammation, neoplasms, adhesions, hernia, volvulus, intussusceptions, food blockage or compression from outside the intestine
- Paralytic ileus, vascular problems, such as mesenteric embolus and thrombus, hypokalemia from diuretics or antihypertensive agents also may result in small bowel obstructions
- Cancer accounts for about 80% of obstructions of the large intestine, with mostly occurring in the sigmoid colon. Other causes are diverticulitis, ulcerative colitis, and previous abdominal surgery. Factors that are caused are mechanical, neurogenic or vascular.
RISK FACTORS
- Mechanical factors: a physical block to passage of intestinal contents without disturbing blood supply of bowel. High small bowel, or low small bowel obstructions occur four times more frequently than chronic obstructions. These includes:
Extrinsic
- Adhesions: these fibrous bands of scar tissue can become looped over a portion of the bowel. The loops then can become either the focus around which the bowel can twist or the band that mechanically obstructs the bowel by external pressure. The presence of multiple adhesions increases the risk of obstruction
- Hernia: an incarcerated hernia may or may not cause obstruction, depending on the size of the hernia ring. However, the potential for obstruction is always present in any hernia. A strangulated hernia is always obstructed because the bowel cannot function when its blood supply is cut-off.
- Volvulus: volvulus is a twisting of the bowel that commonly occurs about a stationary focus in the abdominal cavity. It can cause infraction of the bowel and can occur in either the large or small bowel. Volvulus sometimes can be corrected without surgical interventions. Successful decompression of the bowel with a long tube releases pressure against the proximal end of the loop, thus allowing bowel volvulus to relax
Intrinsic
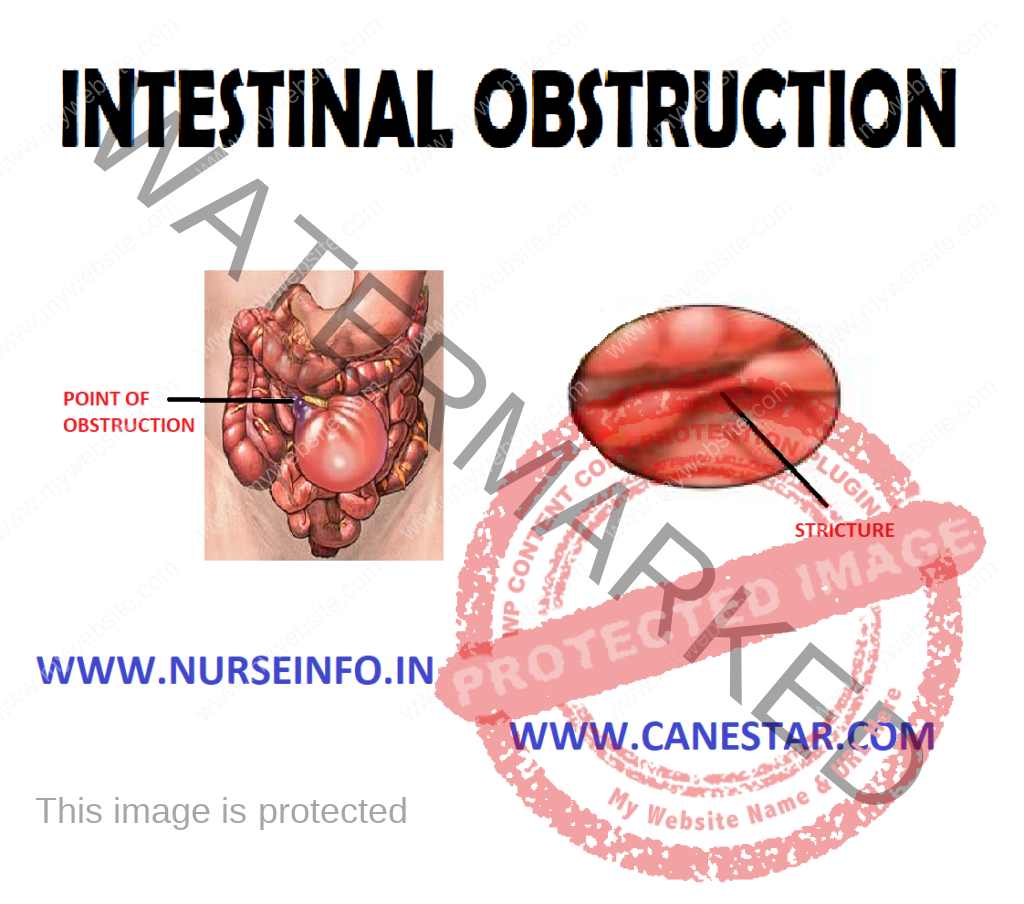
Hematoma, tumor, intussusception (relescoping of intestinal wall inside itself), stricture or stenosis, congenital (artesia, imperforate anus), trauma, inflammatory disease (ulcerative colitis, diverticulum)
Non-mechanical Factor
- Neurologic factors: neurogenic factors are responsible for a dynamic obstruction, also called paralytic ileus, which is caused by lack of peristaltic activity and commonly occurs after abdominal surgery. Extensive surgical procedures in the bowel and in the retroperitoneal area may cause a postoperative neurologic problem. Treatment involves aspiration of secretions by NG suction until the bowel begins to function
- Vascular factors: when the blood supply to any part of the body is interrupted, the part ceases to function and pain occurs. Blood is supplied by way of the celiac and superior and inferior mesenteric arteries. These vessels have autosomotic intercommunications at the head of the pancreas and along the transverse bowel. Obstruction of blood flow can arise as a result of complete occlusion (mesenteric infarction) or partial occlusion (abdominal angina).
- Intraluminal: foreign body, fecal or barium impaction, polyp, gallstones, meconium in infants. In postoperative patients, approximately 90% of mechanical obstructions are due to adhesion.
Other Causes
- Spinal cord injuries, vertebral fractures
- Postoperatively after any abdominal surgery
- Peritonitis, pneumonia
- Wound dehiscence
- GI tract surgery
- Strangulation – obstruction comprises blood supply, leading to gangrene of the intestinal wall, caused by the prolonged mechanical obstruction
TYPES
It is a series that depends on the region of bowel that is affected, the degree to which the lumen is occluded and the degree to which the blood circulation in the bowel wall is disturbed. Treatment involves aspiration of the secretion which involves aspiration of the secretion by gastric suction until the bowel begins to function
- Partial occlusion
- Complete occlusion
Complete Occlusion: an occlusion of arterial blood supply to the bowel as in mesenteric thrombosis effectively stops bowel function. The usual cause is an embolus. The extent of the resulting symptoms is determined by:
- Size of the vessels that is occluded
- The length of the bowel that is without a supply of blood
- The rapidity with which the occlusion occurs
SIGNS AND SYMPTOMS
- Crampy pain that is wave-like and colicky in character
- The patient may pass blood and mucus but no fecal matter and no flatus
- Vomiting
- Obstruction
- Crampy, lower abdominal pain
- Fecal vomiting
- Shock
- Constipation
- Abdominal distension
DIAGNOSTIC EVALUATION
- X-ray studies: abdominal X-ray will show abnormal qualities of gas or fluid in the bowel.
- Lab studies: complete blood cell count, electrolytes, and blood urea nitrogen will reveal dehydration and loss of plasma volume and possibly infection. An elevated WBC count will indicate strangulation or perforation
- Hematocrit: this will indicate hemoconcentration, decreased hemoglobin and HCT values indicate bleeding from neoplasm or strangulation with necrosis. Increased BUN will indicate dehydration, stool to be checked for occult blood
PATHOPHYSIOLOGY
Due to any mechanical or nonmechanical cause —- intestinal content, fluid and gas accumulate above the intestine —- the abdominal distension and retention of fluid reduce the absorption of fluids and stimulate more gastric emptying —- with increasing distension, pressure within the intestinal lumen increases, causing a decrease in venous and arteriolar capillary pressure —- this causes edema, congestion, necrosis, and eventual rupture or perforation of intestinal wall, with resultant peritonitis —- this may lead to vomiting due to abdominal distention —- vomiting may lead to loss of hydrogen ions and potassium from the stomach, reduction of chlorides and potassium in blood and metabolic alkalosis —- excessive loss of water leads to acidosis and that all results in small bowel obstruction
MANAGEMENT
Assessment
- Assess the signs and symptoms of abdominal pain, indigestion, nausea and vomiting
- Take the history of prolonged constipation and complaint of dysphagia and abdominal pain
- Assess for the diagnostic studies of the radiography of the flat and upright abdomen.
- Assess for the abdominal distension through bowel sounds
Decompression of the bowel through a nasogastric tube by the removal of gas, and fluid, correction and relief of the obstruction
Decompression of the bowel is done by inserting the NG tube or intestinal tube
Surgical Management
Surgical management involves resection of the obstructed segment of bowel anastomosing the remaining healthy bowel. Partial or total colectomy, colostomy or ileostomy may be required when extensive obstruction or necrosis is present, e.g. hernia and adhesions.
Nonsurgical Treatment
- Introducing colonoscope for the removal of polyps, dilated strictures, and removing necrotic tumors with laser
- Correction of fluid and electrolyte imbalances with normal saline or Ringer’s solution with potassium as required
- NG suction to decompress bowel
- Treatment of shock and peritonitis
- TNP may be necessary to correct protein deficiency from chronic obstruction, paralytic ileus, or infection
- Analgesics and sedatives, avoiding opiates due to GI mobility inhibition
- Ambulation for the patients with paralytic ileus to encourage return of the peristalsis
NURSING MANAGEMENT
Nursing Diagnosis
- Ineffective breathing pattern related to abdominal distension, interfering with normal lung expansion
- Acute pain related to obstruction, distension and strangulation
- Risk for fluid deficit volume related to impaired fluid intake, vomiting, and diarrhea from intestinal obstruction
- Risk for electrolyte imbalance related to suctioning
- Diarrhea related to obstruction
- Risk of injury related to complication and severity of illness
- Fear related to life-threatening symptoms of intestinal obstruction
- Ineffective breathing pattern related to abdominal distension, interfering with normal lung expansion
Interventions
- Keep the patient in Fowler’s position to promote ventilation
- Provide oxygenation to the patient
- Monitor ABG level for oxygenation to decompress
- Acute pain related to obstruction, distension and strangulation
Interventions
- Provide supportive care during NG intubation to assist with discomfort
- To relieve air-fluid syndrome, turn the patient from supine to prone position every 10 minutes until enough flatus is passed to decompress the abdomen
- A rectal tube may be indicated
- Administer prescribed analgesics
- Risk of fluid deficit volume related to impaired fluid intake, vomiting and diarrhea from intestinal obstruction
Interventions
- Measure and record all intake and output
- Administer IV fluid and parental nutrition as prescribed
- Monitor electrolytes, urine analysis, haemoglobin and blood cells count and report any abnormalities
- Monitor renal output to assess the renal function and to detect urine retention due to bladder compression by the distended intestine
- Monitor vital signs, a drop in BP may indicate decrease circulatory volume due to blood loss from strangulated hernia
- Risk for electrolyte imbalance related to suctioning
Interventions
- Monitor electrolyte values to identify imbalances
- Monitor vital signs and watch for signs of electrolyte for imbalances such as weakness accompanied by low potassium levels to identify imbalances for prompt treatment
- Give ice chips sparingly if ordered by the physician, melted ice increases electrolyte and hydrochloric acid removal when suctioned from the stomach, and electrolyte imbalance and metabolic alkalosis occur
- Diarrhea related to obstruction
Interventions
- Collect stool sample for test for occult blood if occur
- Maintain adequate fluid balance
- Record and amount of consistency of stools
- Maintain NG tube as prescribed to decompress bowel
- Fear related to life threatening symptoms of intestinal obstruction
Interventions
- Recognize the patient’s concerns and initiate measures to provide emotional support
- Encourage the presence of support person
COMPLICATIONS
- Dehydration due to loss of water, sodium and chloride
- Peritonitis
- Shock due to loss of electrolyte and dehydration
- Death due to shock
HEALTH EDUCATION
- Explain the rational for NG suction, NPO status, and IV fluids initially. Advise the patient to progress diet slowly as tolerated once home
- Advise plenty of rest and slow progression of activity as directed by surgeon or other health care provider
- Teach wound care, if indicated
- Encourage the follow-up directed and to call surgeon or health care provider, if increasing abdominal pain, vomiting, or few occur prior to follow-up