INTERSTITIAL LUNG DISEASE – Etiology, Risk Factors, Pathophysiology, Diagnostic Evaluations, Management and Complications
Introduction
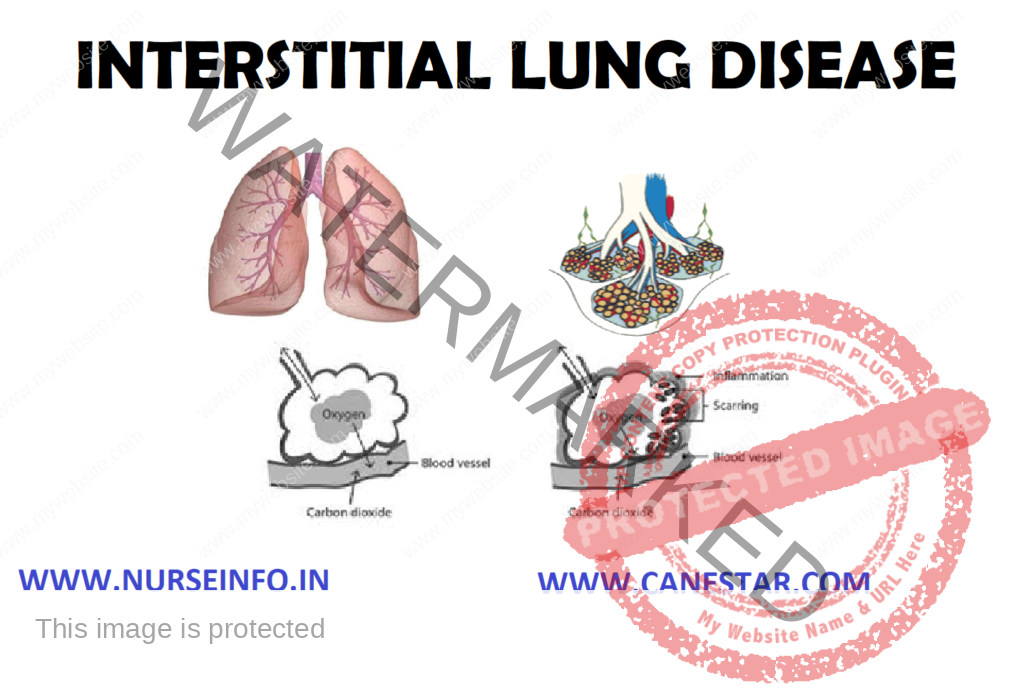
Interstitial lung disease describes a large group of disorders, most of which cause progressive scarring of lung tissue. The scarring associated with interstitial lung disease eventually affects ability to breathe and get enough oxygen into the bloodstream. It can be caused by long-term exposure to hazardous materials, such as asbestos. Some types of autoimmune diseases, such as rheumatoid arthritis, also can cause interstitial lung disease. In most cases, however, the causes remain unknown.
DEFINITION
Interstitial lung disease refers to inflammation in the interstitial tissue of the lungs, the spaces that surround and separate the air sacs.
Types of Interstitial Lung Disease
- Interstitial pneumonia: bacteria, viruses, or fungi may infect the interstitium of the lung. A bacterium called Mycoplasma pneumonia is the most common cause.
- Idiopathic pulmonary fibrosis: a chronic, progressive form of fibrosis of the interstitium. Its cause is unknown.
- Nonspecific interstitial pneumonitis: interstitial lung disease that is often present with autoimmune conditions (such as rheumatoid arthritis or scleroderma)
- Hypersensitivity pneumonitis: interstitial lung disease caused by ongoing inhalation of dust, mold, or other irritants
- Cryptogenic organizing pneumonia (COP): pneumonia-like interstitial lung disease but without an infection present. COP is also called bronchiolitis obliterans with organizing pneumonia (BOOP)
- Acute interstitial pneumonitis: a sudden, severe interstitial lung disease, often requiring life support
- Desquamative interstitial pneumonitis: an interstitial lung disease that is partially caused by smoking
- Sarcoidosis: a condition causing interstitial lung disease along with swollen lymph nodes, and sometimes heart, skin, nerve, or eye involvement
- Asbestosis: interstitial lung disease caused by asbestos exposure
- Silicosis: silicosis is a condition caused by inhaling too much silica over a long period of time. Salica is a crystal-like mineral found in sand and rocks, such as granite. Silica can have deadly consequences for people who work with stone, concrete, glass, or other forms of rock
- Pneumoconiosis: pneumoconiosis, also known as Black Lung Disease, is an occupational lung disease caused by inhaling coal dust
ETIOLOGY
Interstitial lung disease can be triggered by many different things, including airborne toxins in the workplace, drugs and some types of medical treatments. In most cases, the causes are unknown.
- Occupational and environmental factors: long-term exposure to a number of toxins and pollutants can damage your lungs. These may include:
Silica dust
Asbestos fibers
Grain dust
Bird and animal droppings
- Radiation treatments: some people who receive radiation therapy for lung or breast cancer show signs of lung damage months or sometimes years after the initial treatment. The severity of the damage depends on:
How much of the lung was exposed to radiation
The total amount of radiation administered
Whether chemotherapy also was used
The presence of underlying lung disease
- Medications: many drugs can damage your lungs, especially:
Chemotherapy drugs: methotrexate and cyclophosphamide
Heart medications: amiodarone (cordarone) and propranolol
Some antibiotics: nitrofurantoin and sulfasalazine
- Medical conditions: lung damage can also result from:
Systemic lupus erythematosus
Rheumatoid arthritis
Sarcoidosis
Scleroderma
- Unknown causes: the list of substances and conditions that can lead to interstitial lung disease is long. Even so, in most cases, the causes are never found. Disorders without a known cause are grouped together under the label idiopathic pulmonary fibrosis or idiopathic interstitial lung disease
RISK FACTORS
- Age: interstitial lung disease is much more likely to affect adults, although infants and children sometimes develop the disorder
- Exposure to occupational and environmental toxins: if clients working in mines, farming or construction or for any reason are exposed to pollutants known to damage lungs, risk of interstitial lung disease greatly increases.
- Smoking: some forms of interstitial lung disease are more likely to occur in people with a history of smoking, and active smoking may make the condition worse
- Radiation and chemotherapy: having radiation treatments to chest or using some chemotherapy drugs makes it more likely that will develop lung disease
- Oxygen: continually inhaling very high levels of therapeutic oxygen for more than 48 hours can harm the lungs
PATHOPHYSIOLOGY
Acute injury to the pulmonary parenchyma —- leading to chronic interstitial inflammation —- fibroblast activation and proliferation —- progressing to the common endpoint of pulmonary fibrosis —- tissue destruction
SIGNS AND SYMPTOMS
- Shortness of breath
- Dry cough
- Cyanosis
- Clubbing (a painless enlargement of the fingertips)
- Enlarged heart
- Weight loss
- Loss of appetite
- Muscle and joints pain
- Fatigue
DIAGNOSTIC EVALUATION
- Medical history and physical examination
- Blood tests: may help provide direction in the initial stage of diagnosis and rule out other conditions that may have similar symptoms. Measurements of the oxygen level in the arterial blood may also be performed.
- Chest X-ray: a simple chest X-ray is the first test in the evaluation of most people with breathing problems. Chest X-rays films in people with interstitial lung disease may allow fine lines in the lungs
- Computed tomography (CT scan): A CT scanner takes multiple X-rays of the chest and a computer creates detailed images of the lungs and surrounding structures. Interstitial lung disease can usually be seen on a CT scan
- High-resolution CT scan: If interstitial lung disease is suspected, using certain CT scanner settings can improve the images of the interstitium
- Pulmonary function testing: a person sits in a sealed plastic booth and breathes through a tube. PFTs are noninvasive tests that measure the function of the lungs. The test involves blowing into a tube that is part of an instrument called a spirometer. This can measure the volume of the lungs as well as the air flow into and out of the lungs. People with interstitial lung disease may have a reduced total lung capacity. They may also have a decreased ability to transfer oxygen from their lungs into their blood
- Bronchoscopy: an endoscope is advanced through the mouth or nose into the airways. Tiny tools on the endoscope can take a sample of lung tissue
- Video-assisted thoracoscopic surgery (VATS): using tools inserted through small incisions, a surgeon can sample multiple areas of lung tissue
- Lung biopsy: obtaining lung tissue to examine under a microscope is the only way to determine which type of interstitial lung disease a person has. There are several ways to collect lung tissue, which is called a lung biopsy
- Open lung biopsy (thoracotomy): in some cases, traditional surgery with a large incision in the chest is needed to obtain a lung biopsy
MANAGEMENT
- Inhaled oxygen: in people with low oxygen blood levels due to interstitial lung disease, inhaled oxygen may improve symptoms. Regular use of oxygen might also protect the heart from damage caused by low oxygen levels
- Antibiotics: these are effective treatments for most interstitial pneumonias, e.g. azithromycin and levofloxacin eliminate the bacteria that cause most interstitial pneumonias
- Vaccines: influenza vaccine and pneumococcal pneumonia vaccine
- Corticosteroids: in some forms of interstitial lung disease, ongoing inflammation in the lungs causes’ damage and scarring, e.g. prednisone and methylprednisolone reduce the activity of the immune system. This reduces the amount of inflammation in the lungs and the rest of the body.
- Immune-suppressing drug: such as azathioprine or cyclophosphamide are also given, either in combination with steroids or following a course of steroid treatment
- Smoking cessation: it is critical for those with interstitial lung disease
SURGICAL MANAGEMENT
Lung transplant: in advanced interstitial lung disease causing severe impairment, a lung transplant may be the best option. Most people undergoing lung transplant for interstitial lung disease make large gains in quality of life and their ability to exercise
COMPLICATIONS
- Pulmonary hypertension: unlike systemic high blood pressure, this condition affects only the arteries in lungs. It begins when scar tissue restricts the smallest blood vessels, limiting blood flow in lungs. This, in turn, raises pressure within the pulmonary arteries. Pulmonary hypertension is a serious illness that becomes progressively worse
- Right-sided heart failure (Cor pulmonale): this serious condition occurs when right ventricle of heart which is less muscular than the left has to pump harder than usual to move blood through obstructed pulmonary arteries. Eventually the right ventricle fails from the extra strain
- Respiratory failure: in the end-stage of chronic interstitial lung disease, respiratory failure occurs when severely low blood oxygen levels along with rising pressures in the pulmonary arteries and the right ventricle cause heart failure