HIGH ALTITUDE PULMONARY EDEMA – Pathophysiology, Clinical Features, Diagnosis, Treatment and Prevention
This is a more serious complication compared to AMS. Young subjects in apparently good health are more affected. It may manifest in newcomers and also in subjects acclimatized to high altitudes, if they ascend the heights rapidly after long periods of stay at lower altitude. Altitudes above 2500 m can be harmful, but most of the cases occur at heights of 3050 to 4550 m. Heavy meal, physical exertion and too rapid an ascent precipitate the condition. Symptoms start within 6 to 48 hours of reaching the station.
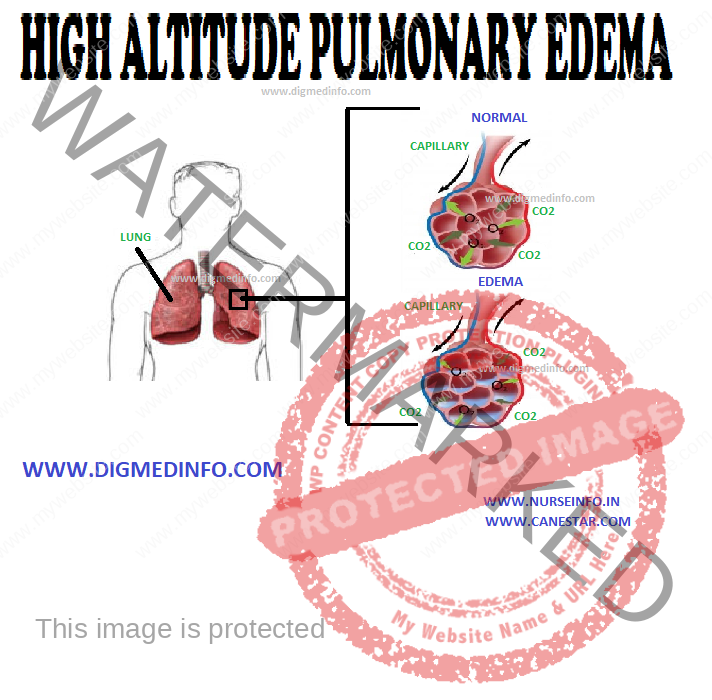
Pathophysiology
Though pulmonary hypertension is invariably found as a consequence of hypoxia, only a small proportion of subjects develop acute pulmonary edema. High-altitude pulmonary edema is a noncardiogenic pulmonary edema associated with pulmonary hypertension and elevated capillary pressure. The pulmonary hypertension is secondary to the exaggerated pulmonary vasoconstriction induced by hypoxia. Sympathetic over activity, endothelial dysfunction, and hypoxemia are the proposed mechanisms. An immunogenetic basis also has been suggested because of higher incidence of HLA-DR6 and HLA-DQ4 antigens in susceptible individuals.
CLINICAL FEATURES
Many cases follow acute mountain sickness, but in some, pulmonary edema develops abruptly. Early symptoms are cough, tachypnea, dyspnea, and chest pain. These are soon followed by hemoptysis, cyanosis, frothy expectoration, and intense chest discomfort. Oliguria may develop.
The course is variable. In some, the pulmonary edema worsens while in others it may become sub acute and persist for a few days. In severe cases right-sided heart failure may follow and this may precede death.
Radiographic abnormalities include prominence of the pulmonary arteries, irregular patchy infiltration of one lung or bilateral nodular densities. Electrocardiogram reveals acute right ventricular strain due to pulmonary hypertension.
Diagnosis
High altitude pulmonary edema should be anticipated in healthy subjects who develop vague cerebral and respiratory symptoms on reaching high altitudes. Early recognition and treatment are necessary to avoid rapid deterioration or cardiac failure. Malingering has to be differentiated from this condition.
Treatment
Immediate treatment under field conditions is rest and administration of 100% oxygen at a rate of 4-6L/min for 15-30 min. Recompression using a portable hyperbaric bag will reduce symptoms if immediate descent is not possible. If oxygen is not available the patient should be evacuated to a lower camp, hospitalized and administered oxygen. Frusemide 40 mg should be given intravenously. Persistence of pulmonary edema is an indication for repeating frusemide. Nifedipine 10 mg initially followed by 20 mg repeated every 12 hours gives symptomatic relief. Physiological venesection by applying tourniquets proximally to the limbs helps to reduce pulmonary edema. Precipitating factors such as respiratory infection have to be looked for and treated appropriately.
Cases, which do not respond to the resuscitatory measures, should be evacuated to lower altitude urgently to prevent death.
Prevention
Proper training and conditioning for 1-2 weeks should be undertaken before reaching high altitudes. Ascent should be gradual to permit acclimatization. On reaching high altitudes, all unacclimatized persons should avoid physical exertion for 48-72 hours. Salmeterol inhalation 125 mg every 12 hours beginning 24 hours before the ascent is recommended to reduce incidence of high altitude pulmonary edema. Nifedipine 20 mg administered as a slow release preparation 8 h is also effective in preventing high attitude pulmonary edema. Those planning to ascent 3000 m should carry supply of oxygen and equipment sufficient for several days.