GLOMERULONEPHRITIS – Etiology, Types, Pathophysiology, Signs and Symptoms, Diagnostic Evaluation and Management
INTRODUCTION
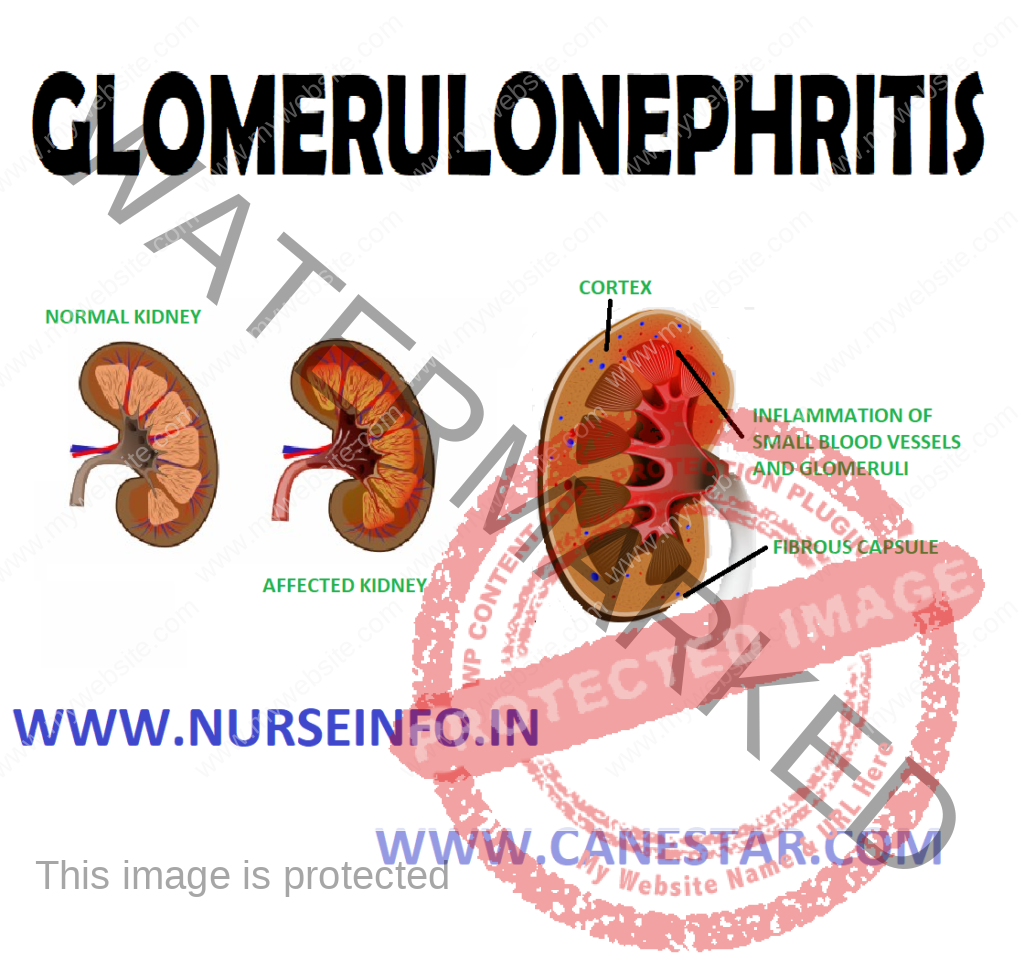
Immunological processes involving the urinary tract predominantly affect the renal glomerulus, the disease process results in glomerulonephritis. It means inflammation of glomeruli, which affects both kidneys equally. It is a type of kidney disease in which the part of kidney (glomeruli) that helps in filter waste and fluids from blood is damaged.
DEFINTION
Glomerulonephritis means inflammation of glomeruli. It is an inflammation of tiny filters of kidney (glomeruli) that helps to remove excess fluid, and waste from bloodstream and pass them into the urine
TYPES
It is of two types acute glomerulonephritis and chronic glomerulonephritis
ACUTE GLOMERULONEPHRITIS
It means active inflammation in glomeruli. Acute glomerulonephritis is most common in children and young adults, but all ages can be affected.
Each kidney is composed of about 1 million filtering screens called glomeruli that remove uremic waste products. The inflammatory process usually begins with the immune system fights off the infection scars tissue forms
There are many diseases that cause an active inflammation within glomeruli. When there is active inflammation occur within the kidney scar tissue may replace normal functional kidney tissue and cause irreversible renal impairment
ETIOLOGY
It is caused when there is problem with immune system or diseases like HIV and lupus that affect immune system. Disorders that attack several organs and can cause glomerulonephritis
It occurs after an infection elsewhere in the body or may develop secondary to systemic disorders
An infection with group A streptococci bacteria
PATHOPHYSIOLOGY
Due to etiological factors, antigen (group A beta hemolytic streptococcus) —- throat infection —- deposition of antigen antibody complex in glomerulus —- increased production of epithelial cells lining the glomerulus —- leukocytes infiltrate the glomerulus —- thickening of the glomerular filtration membrane —- scarring and loss of glomerular filtration membrane —- decreased glomerular filtration rate
SIGNS AND SYMPTOMS
The primary presenting feature of acute glomerulonephritis is hematuria. The urine may be cola, coffee colored because of RBCs and protein plugs
- Proteinuria and elevated (BUN) blood urea and nitrogen and serum creatinine
Other Manifestations
- Oliguria
- Edema fever
- Shortness of breath or dyspnea. Possible flank pain
- Nausea and vomiting
- Abdominal pain
- Back pain, fatigue, weight gain
- Headache, loss of appetite
- Weakness, fatigue
- High blood pressure
DIAGNOSTIC EVALUATION
- History: assess and collect history from patient regarding change in pattern of urination frequency, color or volume
Ask patient for signs and symptoms like headache, nausea, vomiting and loss of appetite
Ask for any history of flank pain
Physical examination: in physical examination assess for adequate intake output
Check vital signs
Monitor weight of patient
Assess patient for edema and any signs and symptoms of infection
- Urinalysis: for the presence of hematuria. A urinalysis may show red blood cells in urine an indicator of damage to the glomeruli. Urinalysis results may also show white blood cells, a common indicator of infection and inflammation and increased protein which results nephron damage.
- Check patient BUN and serum creatinine level. There is an increase in BUN and serum creatinine level
- Needle biopsy: it reveals obstruction of glomerular capillaries from proliferation of endothelial cells. It is a diagnostic test that involves collecting small pieces of tissue, usually through a needle, for examination with a microscope. In this we collect a sample of kidney tissue, to check any unusual deposits, scarring, or infecting organisms that would explain a person’s condition
MANAGEMENT
- Management includes:
Antihypertensive’s to treat high blood pressure and diuretics, they increase the renal blood flow by decreasing renal vascular resistance.
Provide antibiotics if infection is still present usually penicillin. Helps to reduce infection and prevent further spread of infection
Steroids and other medicines will suppress the immune system. Prednisolone and methylprednisolone is useful and most commonly prescribed drug. It can suppress the inflammatory response in kidney and reduce the permeability of renal blood vessels and reducing the proteinuria
Nutritional Therapy
Dietary protein should be restricted if BUN level is increased
Potassium and sodium should be avoided if edema is present
Dietary protein should be restricted if there is evidence of an increase in nitrogenous wastes
Fluid intake should be restricted
Provide low protein diet to the patient
Provide vegetables, rice, cereals, dried beans, breads
Advise to avoid animal products they are rich source of protein
Eat healthy foods
Get proper rest and sleep


Nice