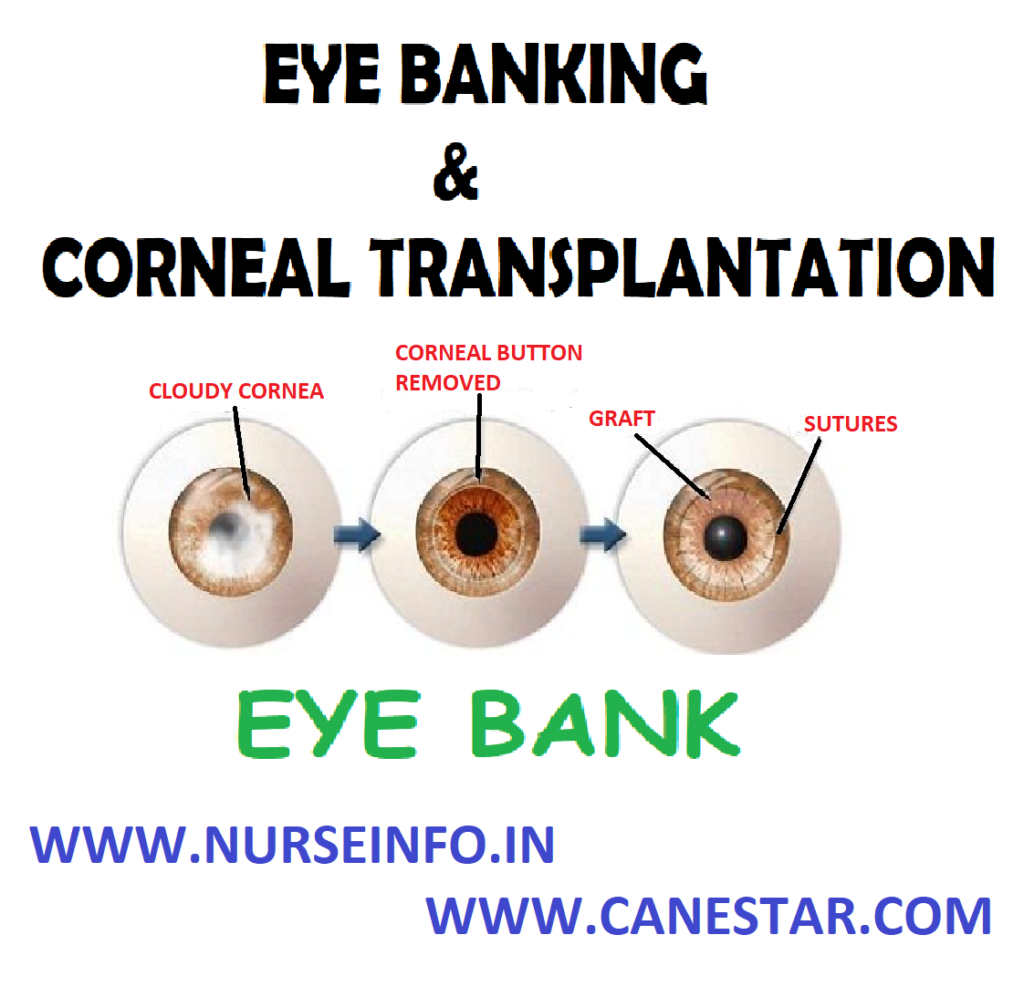
EYE BANKING AND CORNEAL TRANSPLANTATION STEPS OR PROCEDURE
FUNCTIONS OF EYE BANK, CONTRAINDICATIONS FOR DONATION, RETRIEVAL PROCEDURE, ROLE OF NURSE DURING CORNEAL TRANSPLANTATION, AFTER SURGERY and HOME CARE INSTRUCTIONS
It is an organization that deals with the collection, storage and distribution of donor eyes for the purpose of corneal grafting
- Corned blindness is a major form of visual deprivation in developing countries. A high percentage of these individuals can be visually rehabilitated by corneal transplantation (keratoplasty), a procedure that has very high rate of success among organ transplants. Quality of donor cornea, the nature of recipient pathology and the availability of appropriate postoperative care are the factors that determine the final outcome of this procedure. In corneal grafting, this diseased and opaque cornea is replaced by a healthy transplant cornea taken from a donor eye.
- A corneal transplant can take one of two forms: a full-thickness penetrating keratoplasty, involving excision and replacement of the entire cornea, or a lamellar keratoplasty, which removes and replaces a superficial layer of corneal tissue.
FUNCTIONS OF EYE BANK
Procurement and supply of donor cornea to the corneal surgeons is the primary goal of eye banks.
- The eye bank collects the eyes of voluntary registered eye donors after their death of those deceased person when enlightened relatives agree to donate the eyes as a service to humanity. From hospital deaths and from postmortem cases, after obtaining the consent from the next of kin.
- These eyes are processed by the Eye Bank and are supplied to eye surgeons for corneal grafting and other sight restoring operations
- Before proceeding for recovery eye bank personnel should ascertain the following details: location, age of the donor, cause of death and time of death.
CONTRAINDICATIONS FOR DONATION
- All eye banks have age limits both minimum and maximum
- Previous corneal graft
- Death of unknown cause
- Dementia
- Creutzfeldt-Jacob disease
- Subacute sclerosing panencephalitis
- Congential rubella
- Reyes syndrome
- Active viral encephalitis or encephalitis of unknown origin
- Active septicemia
- Rabies
- Retinoblastomas, tumors of the anterior segment
- Active ocular infections
- Pterygia or other superficial disorders of the conjunctiva or corneal surface
- Certain intraocular or anterior segment surgeries
- Leukemia
- Active disseminated lymphomas
- Hepatitis B and C, HTLV-1 or 2, HIV, syphilis
- Behavioral and or social issues, i.e. homosexual or other high-risk sexual behavior within the last 5 years
- Intravenous drug use for nonmedical reasons within the last 5 years
- Exposure to infectious disease within the last year by contact with an open wound, needle stick, or mucous membrane
- Tattooing or piercing within the last 12 months using shared instruments
RETRIEVAL PROCEDURE
- Retrieval procedure could be either enucleation or corneal scleral rim excision
- Eye Bank team on arrival at the location should locate the next of kin and convey condolence and obtain death certificate
- In the absence of a death certificate the registered medical practitioner should satisfy self that life is extinct
- The eye bank team should obtain consent on a consent form from the legal custodian of the donor
- After obtaining consent the donor should be identified either through a tag or through the next of kin
- The eye bank team should then proceed to prepare the site
- Gross physical examination should be conducted with utmost respect for observations regarding build: average, healthy or emaciated
- Eye bank team should look out for needle marks on the arm, skin lesions, etc
- Eye bank team should look out for ulcers or gangrene in exposed areas
- Ocular examination should be conducted
- Medical records and medical information should be obtained
- Information for hemodilution should be obtained
- Social history of the donor should be obtained wherever possible from the next of kin
ROLE OF NURSE DURING CORNEAL TRANSPLANTATION
- Explain the transplant procedure to the patient and answer any questions he may have
- Advise him that healing will be slow and that his vision may not be completely restored until the sutures are removed, which may be in about a year
- Tell the patient that most corneal transplants are performed under local anesthesia and that he can expect momentary burning during injection of the anesthetic
- Explain to him that the procedure will last for about an hour and that the he must remain still until it has been completed
- Tell the patient that analgesics will be available after surgery because he may experience a dull aching
- Inform him that a bandage and protective shield will be placed over the eye
- As ordered, administer a sedative or an osmotic agent to reduce intraocular pressure
- Ensure that the patient has signed a consent form
AFTER SURGERY
- After the patient recovers from the anesthetic, assess for and immediately report sudden, sharp, or excessive pain, bloody, purulent, or clear viscous drainage or fever
- As ordered, instill corticosteroid eyedrops or topical antibiotics to prevent inflammation and graft rejection
- Instruct the patient to lie on his back or on his unaffected side, with the bed flat or slightly elevated as ordered. Also, have him avoid rapid head movements, hard coughing or sneezing, bending over, and other activities that could increase intraocular pressure; likewise, he should not squint or rub his eyes
- Remind the patient to ask for help in standing or walking until he adjusts to changes in his vision
- Make sure that all his personal items are within his field of vision
HOME CARE INSTRUCTIONS
- Teach the patient and his family to recognize the signs of graft rejection (inflammation, cloudiness, drainage, and pain at the graft site)
- Instruct them to immediately notify the doctor if any of these signs occur
- Emphasize that rejection can occur many years after surgery; stress the need for assessing the graft daily for the rest of the patient’s life. Also, remind the patient to keep regular appointments with his doctor
- Tell the patient to avoid activities that increase intraocular pressure, including extreme exertion, sudden, jerky movements, lifting or pushing heavy objects and straining during defecation
- Explain the photophobia, a common adverse reaction, gradually decreases as healing progresses
- Suggest wearing dark glasses in bright light
- Teach the patient how to correctly instill prescribed eyedrops
- Remind the patient to wear an eye shield when sleeping
- Tell the patient to consult with the surgeon before driving or participating in sports or other recreational activities