ENDOTRACHEAL INTUBATION – Definition, Purpose, Assessment Phase, Precautions, Planning Phase, Client/Family Teaching and Equipment Used
DEFINITION
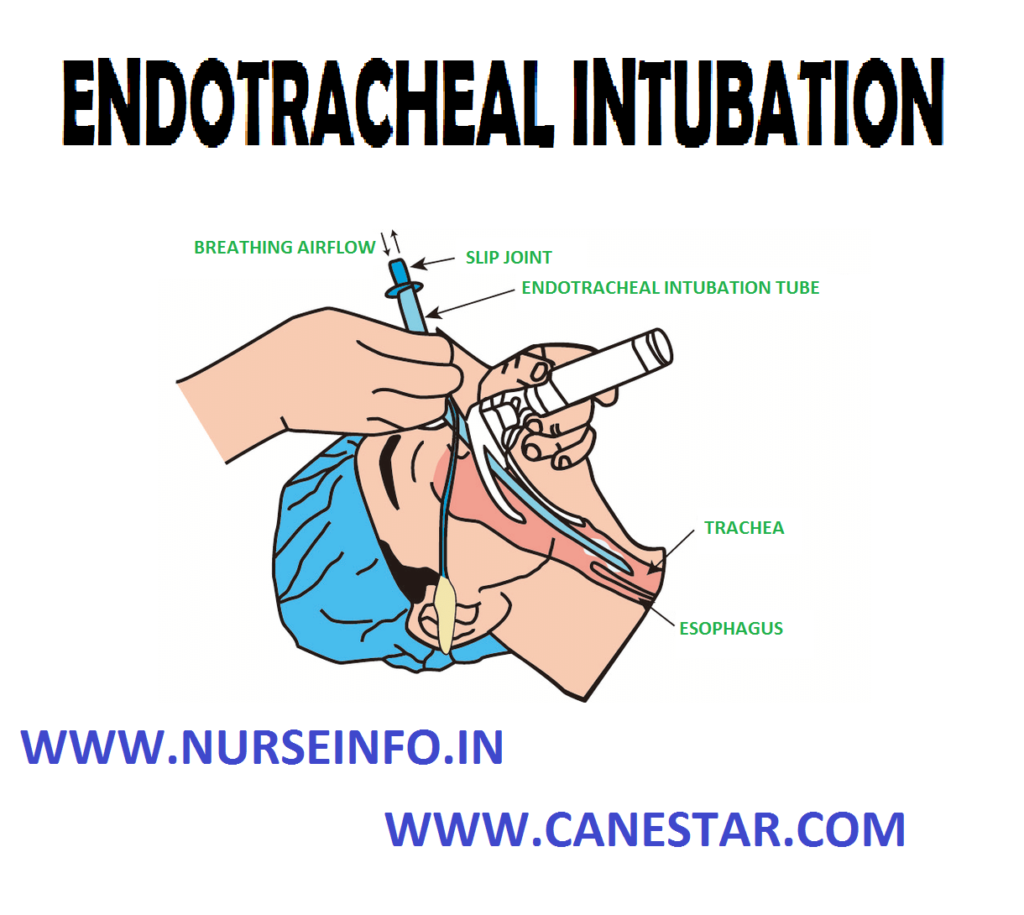
Endotracheal intubation is assisting in passing of a slender hollow tube into trachea through nose or mouth to facilitate artificial ventilation and resuscitation, using aseptic technique
PURPOSE
- To treat acute respiratory failure, persistent hypoxemia, persistent rise in pCO2
- To maintain patient airway
- To ensure adequate oxygenation in fracture of cervical vertebrae, spinal cord injury
- To provide ventilatory assistance when indicated
Objective: to insert an endotracheal tube into the trachea to provide a patient airway for ventilatory support or to manage secretions
ASSESSMENT PHASE
- Does the client require intubations? Why are intubations being considered?
- Based on time consideration and on the condition of the client. Should nasal or oral intubations be attempted?
- Will the client need mechanical ventilation after intubations?
PRECAUTIONS
- Avoid damage to the client’s teeth and soft tissue, which can be caused by improper use of the laryngoscope and tubes or by unnecessary force during the procedure
- Ensure the availability of a oxygen source. Ventilate the client with a manual resuscitator using 100 percent oxygen if intubation cannot be accomplished within a reasonable period
- Have suction equipment setup and operable at the client’s bedside before performing the procedure
- Avoid bronchial intubations by correctly positioning the endotracheal tube above the level of the carina
- Be alert for signs of esophageal intubations. These signs include abdominal distention, belching and lack of breath sounds in the lung fields after intubations
PLANNING PHASE
- Endotracheal tubes with low pressure cuffs in various sizes (most common sizes for adult client range from 5 to 9 mm inside diameter)
- Laryngoscope handle and several sizes of both curved and straight blades
- Topical anesthetic spray and sedative
- Water-soluble anesthetic lubricating jelly
- Flexible stylet
- Forceps
- 10 ml syringe
- Oral airway or bite block
- Tape, benzoin tincture and alcohol swabs
- Suction equipment
- Manual resuscitator with oxygen source
CLIENT/FAMILY TEACHING
- If the client is conscious, explain the need for endotracheal intubations and explain the procedure
- Explain sensations that may be experienced during the procedure
- Explain the need for endotracheal intubations and explain the procedure to the family
EQUIPMENT USED FOR ENDOTRACHEAL INTUBATION: IMPLEMENTATION PHASE
- Ensure that client is properly oxygenated using manual resuscitator with 100% oxygen
- Administer medications as ordered
- Check equipment
Use syringe to inflate tube cuff. Check for uniform inflation and leaks before use
Check laryngoscope batteries and light by attaching proper sized blade
- If using stylet, lubricate entire length and insert into endotracheal tube. Make sure tip of stylet does not extend beyond tip of endotracheal tube
- Remove client’s dentures or partial plates if applicable
- Hyperextend client’s neck or place client’s head in brandy sniffing position
- Open client’s mouth using crossed finger technique if necessary. Spray posterior pharynx with topical anesthetic. Suction mouth and pharynx if necessary
- Hold laryngoscope in left hand. Insert blade into right side of client’s mouth, moving to center of mouth to displace tongue
- Advance blade until epiglottis is visualized. If straight blade is used, advance blade past epiglottis. If curved blade is used, position tip of blade anterior to epiglottis in the vallecula
- Lift laryngoscope to a 45 degree angle. Do not use the teeth a pivot
- If oral intubations will be used, insert endotracheal tube through mouth into larynx between vocal cords
- Advance tube until cuff disappears behind vocal cords. If nasal intubations will be used, insert endotracheal tube through nares into the pharynx. Forceps may now be used to guide tube between vocal cords and into larynx. Advance tube until cuff disappears behind vocal cords
- Holding tube in place, removes stylet, if used, and inflate cuff
- Ventilate client with manual resuscitator and 100% oxygen. Auscultate chest during ventilation. Suction endotracheal tube is necessary
- Secure tube with adhesive tape. Before applying tape, wipe client’s cheeks with alcohol and benzoin
- Obtain chest film
- Connect client to oxygen using Briggs adapter or to mechanical ventilator
- Check cuff inflation using pneumometer. Pressure should not exceed 25 cm. record pressure and volume of air required to maintain seal