DISSECTION/DISSECTING AORTA – Definition, Incidence, Classification, Etiology, Pathophysiology, Risk Factors, Diagnostic Evaluation and Management
Introduction
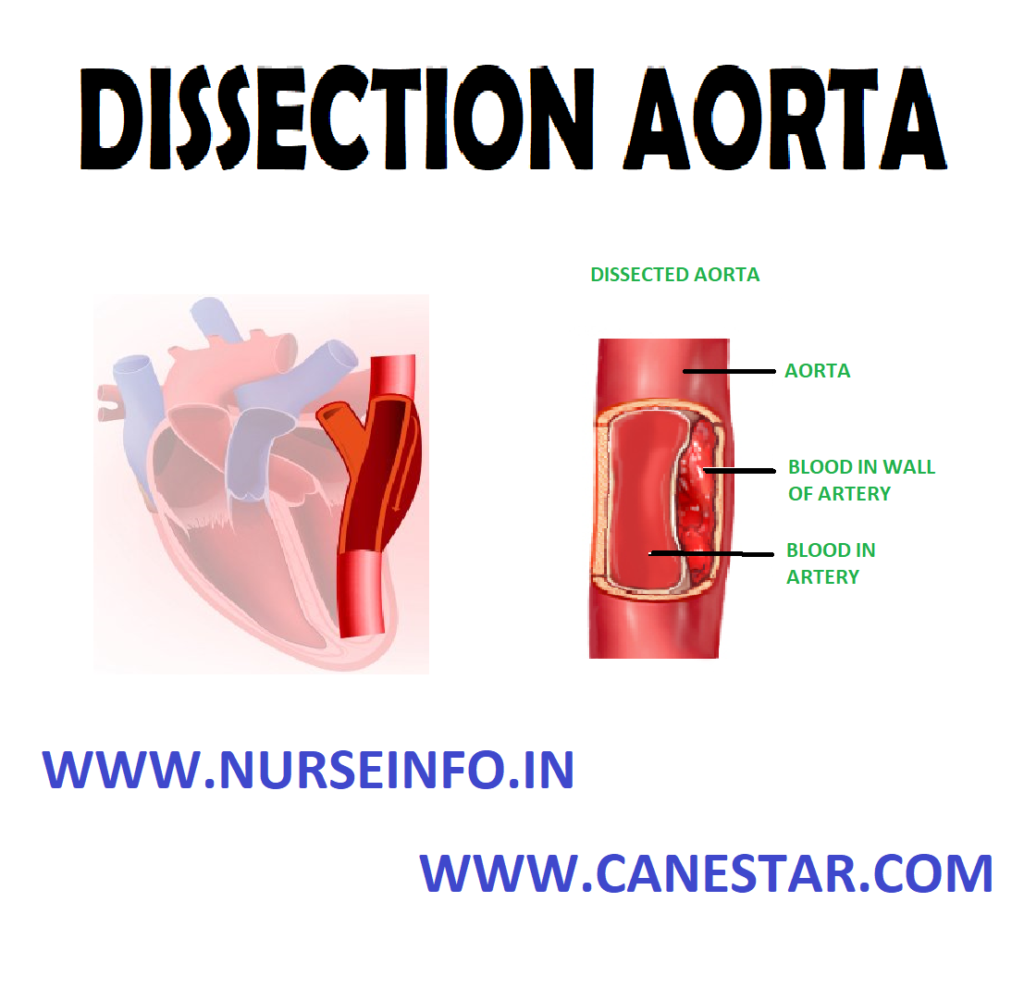
Occasionally, in aorta diseases by atherosclerosis, a tear develops in the intima or the media degenerate, resulting in a dissection.
DEFINITION
An aortic dissection is a serious condition in which a tear develops in the inner layer of the aorta, the large blood vessel branching off the heart. Blood surges through this tear into the middle layer of the aorta, causing the inner and middle layers to separate (dissect). If the blood-filled channel ruptures through the outside aortic wall, aortic dissection is often fatal.
INCIDENCE
Arterial dissection is commonly associated with poorly controlled hypertension. It is 3 times more common in men than in women and occurs most commonly in 50 to 70 year old age group. Dissection is caused by rupture in the intima layer. A rupture may occur through adventitia or into the lumen through intima, allowing blood to re-enter the main channel and resulting in chronic dissection or occlusion of branches of the aorta.
CLASSIFICATION
Stanford Classification
The Stanford classification divides dissections into 2 types, type A and type B. Type A involves the ascending aorta (DeBakey types I and II); type B does not involve (DeBakey type III)
- Type A dissections involve the ascending aorta and arch
- Type B involves the descending aorta
- A patient can have a type A dissection, type B dissection, or a combination of both
DeBakey Classification
The DeBakey system, named after surgeon and aortic dissection sufferer Michael E. DeBakey, is an anatomical description of the aortic dissection. It categorizes the dissection based on where the original intimal tear is located and the extent of the dissection (localized to either the ascending aorta or descending aorta, or involves both the ascending and descending aorta. The DeBakey classification divides dissections into 3 types as follows:
- Type I: originates in ascending aorta, propagates at least to the aortic arch and often beyond it distally. It is most often seen in patients less than 65 years of age and is the most lethal form of the disease.
- Type II: originates in and is confined to the ascending aorta
- Type III: originates in descending aorta, rarely extends proximally but will extend distally. It most often occurs in elderly patients with atherosclerosis and hypertension
ETIOLOGY
- High blood pressure: most cases (over 70%) are associated with high blood pressure (hypertension)
- Bicuspid aortic valve (a congenital abnormality of the aortic valve)
- Marfan’s syndrome
- Ehlers-Danlos syndrome
- Turner syndrome
- Syphilis
- Cocaine use
- Pregnancy: pregnancy is a rare associated risk factor, especially in the third trimester and early in the postpartum period
- Trauma: blunt trauma is known to cause dissection, which is often seen after car wrecks in which the patient’s chest hits the steering wheel
- Surgical complications: operations including coronary artery bypass grafting and aortic and mitral valve repairs. It can also be a complication of heart catheterization
RISK FACTORS
The exact cause is unknown, but more common risks include:
- Aging
- Atherosclerosis
- Blunt trauma to the chest, such as hitting the steering wheel of a car during an accident
- High blood pressure
PATHOPHYSIOLOGY
As the separation progresses —- the arteries branching from the involved area of the aorta shear and occlude —- the tear most commonly occurs in the region of aortic arch —- the dissection of the aorta may progress in backward direction of the heart —- obstructing the opening of coronary arteries —- producing hemopericardium, aortic insufficiency —- it may extend in opposite direction —- occlusion of arteries supplying GI tract, kidneys, spinal cord or legs
CLINICAL MANIFESTATIONS
- Onset of symptoms is sudden
- Severe and persistent pain – anterior chest or back extend to shoulder, epigastric region and abdomen
- Sweating
- Tachycardia
- Appear pale
- Increased blood pressure
The symptoms usually begin suddenly, and include severe chest pain. The pain may feel like a heart attack, and can:
- Be described as sharp, stabbing, tearing, or ripping
- Be felt below the chest bone, then move under the shoulder blades or to the back
- Move to the shoulder, neck, arm, jaw, abdomen, or hips
- Change position – pain typically moves to the arms and legs as the aortic dissection gets worse
The symptoms are caused by a decrease of blood flowing to the rest of the body, and can include:
- Anxiety and a feeling of doom
- Fainting or dizziness
- Heavy sweating (clammy skin)
- Nausea and vomiting
- Shortness of breath – trouble breathing when lying flat (orthopnea)
Other symptoms may include:
- Pain in the abdomen
- Stroke symptoms
- Swallowing difficulties from pressure on the esophagus
ASSESSMENT AND DIAGNOSTIC TESTS
- Physical examination: superficial veins of neck, chest or arm dilated
- D-dimer: a blood D-dimer level less than 500 ng/ml may be able to rule out the diagnosis of aortic dissection alleviating the need for further imaging
- Chest X-ray: widening of the mediastinum on an X-ray of the chest has moderate sensitivity in the setting of an ascending aortic dissection. Pleural effusions may be seen on chest X-ray. They are more commonly seen in descending aortic dissections. Depression of the left main stem bronchus and tracheal deviation
Computed Tomography
Computed tomography angiography is a fast noninvasive test that will give an accurate three-dimensional view of the aorta. These images are produced by taking rapid thin-cut slices of the chest and abdomen, and combining them in the computer to create cross-sectional slices. In order to delineate the aorta to the accuracy necessary to make the proper diagnosis, an iodinated contrast material is injected into a peripheral vein. Contrast is injected and the scan performed using a bolus tracking method. This is a type of scan timed to an injection to capture the contrast as it enters the aorta. The scan will then follow the contrast as it flows through the vessel
It has a sensitivity of 96 to 100% and a specificity of 96 to 100%. Disadvantages include the need for iodinated contrast material and the inability to diagnose the site of the intimal tear.
Magnetic Resonance Imaging
Magnetic Resonance Imaging (MRI) is currently the gold standard test for the detection and assessment of aortic dissection, with a sensitivity of 98% and a specificity of 98%. An MRI examination of the aorta will produce a three-dimensional reconstruction of the aorta, allowing the physician to determine the location of the intimal tear, the involvement of branch vessels, and locate any secondary tears. It is a noninvasive test, does not require the use of iodinated contrast material, and can detect and quantitate the degree of aortic insufficiency.
The disadvantage of the MRI scan in the face of aortic dissection is that it has limited availability and is often located only in the larger hospitals, and the scan is relatively time-consuming. Due to the high-intensity magnetic fields used during MRI, an MRI scan is contraindicated in individuals with metallic implants. In addition, many individuals experience claustrophobia while in the MRI scanning tube
Transesophageal Echocardiography
It is an echocardiogram displaying the true lumen and false lumen of an aortic dissection. In the image to the left, the intimal flap can be seen separating the two lumens. In the image to the right, color flow during ventricular systole suggests that the upper lumen is the true lumen.
The transesophageal echocardiogram (TEE) is a relatively good test in the diagnosis of aortic dissection, with a sensitivity of up to 98% and a specificity of up to 97%. It has become the preferred imaging modality for suspected aortic dissection. It is a relatively noninvasive test, requiring the individual to swallow the echocardiography probe. It is especially good in the evaluation of AI in the setting of ascending aortic dissection, and to determine whether the ostia (origins) of the coronary arteries are involved. While many institutions give sedation during transesophageal echocardiography for added patient comfort, it can be performed in cooperative individuals without the use of sedation. Disadvantages of the TEE include the inability to visualize the distal ascending aorta (the beginning of the aorta arch), and the descending abdominal aorta that lies below the stomach. A TEE may be technically difficult to perform in individuals with esophageal strictures or varices
Aortogram
An aortogram involves placement of a catheter in the aorta and injection of contrast material while taking X-rays of the aorta. The procedure is known as aortography. Previously thought to be the diagnostic ‘gold standard’, it has been supplanted by other less-invasive imaging modalities
MEDICAL MANAGEMENT
- Antibiotic: the antibiotic doxycycline is currently being investigated for use as a potential drug in the prevention of aortic aneurysm due to its metalloproteinase inhibitor and collagen stabilizing properties
- Antihypertensive: hydralazine hydrochloride
- Beta blocker: atenolol, timolol maleate
- Vasodilators: sodium nitroprusside
- Calcium channel blockers: verapamil and diltiazem
SURGICAL MANAGEMENT
Replacement of the damaged section with a tube graft (often made of Dacron) when there is no damage to the aortic valve
- Bentall procedure: replacement of the damaged section of aorta and replacement of the aortic valve
- David procedure: replacement of the damaged section of aorta and reimplantation of the aortic valve
- Tevar: insertion of a stent graft (covered stent): e.g. in TEVAR (thoracic endovascular aortic repair). It is usually combined with ongoing medical management
- Vascular ring connector (VRC): replacement of the damaged section of aorta with a sutureless vascular ring connector-reinforced Dacron graft. Vascular ring connector (VRC) is a titanic ring used as a stent in the vascular graft to achieve a quick, blood-sealed and sutureless anastomosis. There are two furrows on the surface of the ring for fixation of the vascular graft and the aorta. The tapes used to tie against the ring provide a larger contact surface area than the traditional stitches, thus providing stronger anastomosis and better surgical results.