DIABETES MELLITUS – MANAGEMENT (Medical Nutritional Therapy)
Diet is the corner stone in the management of diabetes. The objective of dietary therapy is the optimization of glycemic control and to provide a nutritious and balanced diet. In type 1 DM patients the total energy input has to be relatively higher in order to regain ideal weight and growth. In type 2 patients the calories need to be restricted in order to avoid obesity. Dietary articles such as saturated fats, excess salt and cholesterol which promote vascular complications have to be avoided.
Goals of Medical Nutrition Therapy
1. To achieve and maintain near normal glycemia(euglycemia).
2. To achieve and maintain optimal lipid profile. (total cholesterol < 150, triglyceride ± 120, HDL>50 and LDL<100/mg/dL).
3. To achieve and maintain normal blood pressure levels around 120 to 130 / 80 to 85 mmHg.
4. To adjust the nutrient intake to restore and maintain ideal body weight to avoid dyslipidemia, cardiovascular disease, hypertension and nephropathy. During childhood and pregnancy adjustment for growth also should be provided.
5. For elderly patients, provision for proper nutrition and psychosocial needs.
In type 2 diabetic patients the first step would be dietary therapy alone along with exercise. They should be given a trial of dietary therapy for 4-8 weeks. About 50% of the patients come under control with diet alone. Proper patient education helps to improve adherence to treatment.
The following points have to be considered while prescribing a diet for a diabetic-
1. The type of diabetes- type 1 or type 2
2. The weight of the individual in comparison with his ideal body weight (BMI)
3. His occupation and activities and to assess his caloric requirements
4. The presence of any complications
An appropriate assessment of the caloric needs of each diabetic individual should be done.
Total Caloric Intake
This is the most important step while prescribing a diet. Total caloric intake depends on the patient’s body weight, degree of physical activity and the presence of any other comorbid illnesses. Obesity is an important factor in terms of target cell resistance to insulin action.
The body mass index (BMI) will help to determine the total caloric requirement.
BMI = Weight (in Kg) / Height in m2. It is desirable to keep the BMI between 22 and 25.
Ideal body weight can be readily calculated by the formula: ideal body weight = height in cm – 100.
The recommended daily allowance is 30 Kcal/kg of desirable body weight to patients with average activity except in the case of obesity where appropriate changes have to be made.
Having calculated the number of calories required, they are distributed into at least three principal meals and one or two small snacks. These calories are derived from three principal sources—carbohydrates, protein and fats. Each fraction has its own importance and should provide 60% of the calories from carbohydrates and 20% each from proteins and fats.
When instructing on the diet regime the following points should be stressed.
1. It is not a reduction in the diet; on the other hand it is a modulation to suit the particular need of the individual. This concept will help to reduce the psychological resistance in accepting the diet.
2. The patient and his spouse should be counseled together, so that the latter will understand the principles and help to provide the diet appropriately.
3. Whenever possible, the dietary articles should be prescribed in terms of weight so that at least on a few occasions the actual quantities would be determined and adopted.
4. It is better to prescribe the diet in terms of the primary food articles such as rice, meat, fish and others so that the patient can determine the various items of the menu in relation to the allowed foodstuff.
5. Many patients are under the wrong impression that reducing the food further than what is prescribed may be beneficial and this should be avoided.
6. Both the quantity to diet and its timing are important since other aspects of management such as medication and exercise are timed in relation to the diet. As far as possible the diet should conform to the cultural habits and socioeconomic condition of the patient.
7. Vast majority of treatment failure can be avoided by proper dietary instructions.
8. At all follow-up visits enquiry on the diet should be made and the need for strict adherence stressed.
9. As far as possible the patient should be involved in the formulation of the diet and such a participatory instruction assures better compliance.
Carbohydrates
The amount of carbohydrates to be permitted in diet of diabetic patients has been an area of controversy. Till recently most people recommended restriction of carbohydrates in the diet to provide only 30-40% of the calories. Our diets in India are cereal based and have a high carbohydrate component (about 70%).
The American Diabetic Association and the European Diabetic Association study groups have also altered their dietary recommendations. In an attempt to reduce cardiovascular morbidity and mortality, they now recommend a liberalized use of carbohydrates in the diet up to 50-60% of the calories. This also helps to reduce the intake of saturated fats. Modification in the type of carbohydrate can be achieved by increasing the intake of legumes and pulses, green leafy vegetables and other vegetables, which will increase the content of complex carbohydrates and fiber.
Fats
The fat content of diet should be 20-25% of the total calories. The distribution of the type of fat should be equal, i.e. saturated fats and mono and polyunsaturated fats should be equally distributed to make up the total fat intake. The dietary cholesterol should be less than 300 mg/day. Invisible fat is derived in a fair amount from cereals, legumes and seeds and contributes to 5-10% of the total energy intake. Milk and Milk products contribute approximately to 40-45% of the total fat content in vegetarian diets. Milk fat is a saturated fat.
Proteins
Protein intake has been recommended as 0.8 g/kg body weight and should contribute to 12–20% of the total caloric intake. Vegetable proteins derived from cereals and lentils, do not contain cholesterol. They have high fiber content. Animal protein is rich in saturated fats and tends to increase cholesterol and triglycerides. Lean meat and fish are to be preferred to fatty meat in order to minimize the risk. When renal failure occurs, strict-protein restriction is instituted.
The dietary salt should be less than 6 g/day. In the presence of hypertension or renal failure it should be reduced to around 3 g/day. Alcohol should be avoided as far as possible. Alcohol intake will increase the risk of hypoglycemia by inhibiting gluconeogenesis. It may induce ketoacidosis, lactic acidosis and may contribute to peripheral neuropathy. Alcohol also induces hypertriglyceridemia and hyperuricemia. Alcohol is an additional source of calories, without any further nutritional values each mL providing 7 calories. If consumed it should be taken only in moderate quantities (1-2 drinks/day i.e. 20-40 mL/day).
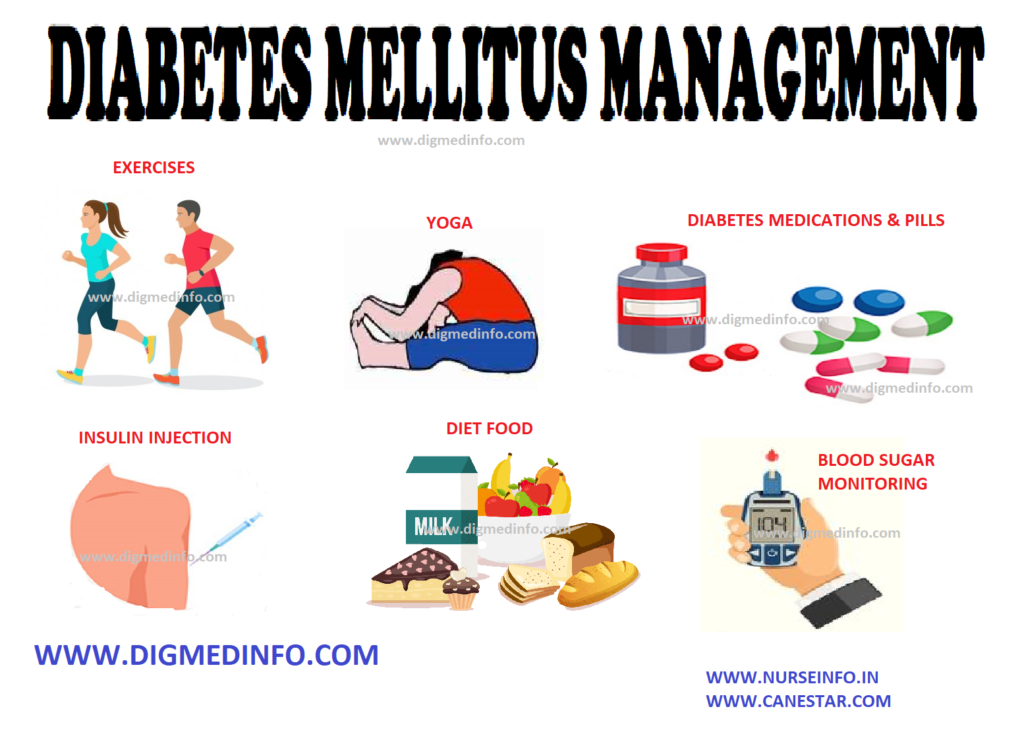
EXERCISE
In type 2 diabetes, regular exercise forms an important component of therapy along with dietary regulation and oral hypoglycemic agents. However a careful assessment of the expected benefits and associated risks of exercise in individual patients should be made while incorporating an exercise program in the treatment. Appropriate monitoring should be done to avoid complications.
Exercise should not be recommended indiscriminately in all type 1 diabetic patients but efforts should be made, to make it possible for those who want to exercise to do so as safely as possible.
Endocrine/Physiological Responses during Exercise
1. Suppression of insulin release – directly as well as through epinephrine.
2. Sympathetic system activation – which inhibits insulin release (by alpha-receptor stimulation) and stimulates lipolysis.
3. Non-insulin dependent glucose uptake in the periphery. In both type 1 and type 2 diabetic patients who are under good control the response to exercise will be normal. In untreated type 1 patients there is an increased production of FFA from adipocyte lipolysis, which leads to decreased glucose uptake in the periphery. This can even precipitate diabetic ketoacidosis in some patients.
In the well-controlled patients this does not occur While prescribing exercise, it should suit the social and economic condition of the patient and his work schedule. Regular exercise as part of the therapeutic intervention should be taken by all diabetics, irrespective of the physical activity entailed in their regular occupation.
Maximum benefit is achieved by exercises such as brisk walking (4-5 km/hour), swimming, cycling and such other aerobic exercises. At least five sessions a week should be performed in order to achieve optimal benefit. While starting the exercise program in persons above the age of 35 years clinical assessment of their cardiovascular status should be done and introduction of the exercise regimen should be gradual, so as not to precipitate any acute cardiovascular events.
For the average middle-aged Indian diabetic the following exercise regimen is adequate.
• Walk 3 km on level ground over a period of 45 minutes
• Swim for 30 minutes at average speed without cardiovascular distress.
• Cycle on level ground at 8 km/hour for 30 minutes.
Regular sports and games activities can be undertaken and should be encouraged by those who desire to do them, with special provision made for the diet and medications. Since such sport activities are likely to be intermittent rather than regular, in practice walking or cycling is more regularly available.
Before an exercise program is initiated, a fair control of blood glucose is to be ensured and a thorough clinical evaluation of the patient should be made particularly in regard to complications of diabetes such as hypertension, coronary artery disease, peripheral vascular disease, retinopathy and nephropathy.
Yoga exercises
Recently several well-planned studies have demonstrated the beneficial effects of yogic practices in diabetics. Patients with diabetes demonstrated a significant fall in fasting and postprandial blood glucose values and HbA1c, with reduction in the requirements of OHA and insulin. Type 1 diabetic patients with brittle diabetes showed marked improvement with the practice of yoga. There was a salutary effect on the lipid profile, with a fall in serum cholesterol, triglycerides and an increase in HDL- cholesterol fraction. Certain Asanas (specific postural manipulations which have to be learnt under supervision) have been identified as useful in the control of diabetes. Thus yogic practices have a useful role in the control of diabetes and prevention of its longterm complications.
ORAL HYPOGLYCEMIC AGENTS (OHAs)
The oral hypoglycemic agents are indicated in type 2 diabetes when diet and exercise fail to achieve euglycemia. The two major groups of drugs in use are a) Insulin secretogogues (sulfony1 urea compounds) and b) insulin sensitizers (glitazones).
Sulphonylurea (SU) Compounds
The SU compounds stimulate the beta cells of the pancreas to release insulin. Therapy should be initiated with the smallest dose, taken 15-30 minutes before breakfast and small increments should be made at weekly intervals till the optimum dose is reached. The sulfonylureas are similar in effectiveness in equipotent doses and in the absence of any specific reason such as adverse side effects, cost or nonavailability, there is no need to change the medication in patients who are adequately controlled. So also there is no advantage in combining two or more sulfonylurea drugs.
INSULIN THERAPY
Therapeutics of Insulin
Insulin therapy aims at providing ideal physiological insulin profiles with peaks at meal times and maintenance of basal levels between meals and at night. This can be achieved by administering soluble insulin before each meal and adding a dose of intermediate acting insulin at bed time. The alternative regimes would be; (i) a split dose of soluble and intermediate acting insulin before breakfast and dinner, (ii). a single dose of soluble and intermediate acting insulin before breakfast, (iii) a single dose of intermediate acting insulin before breakfast. With the introduction of premixed insulin it is easier for the patients to adopt these regimes. As in the case of other hypoglycemic agents, diet control and exercise should be instituted along with insulin therapy.