COR PULMONALE – Etiology, Clinical Manifestations, Diagnostic Evaluations and Management
- Cor pulmonale is a condition that most commonly arises out of complications from pulmonary hypertension
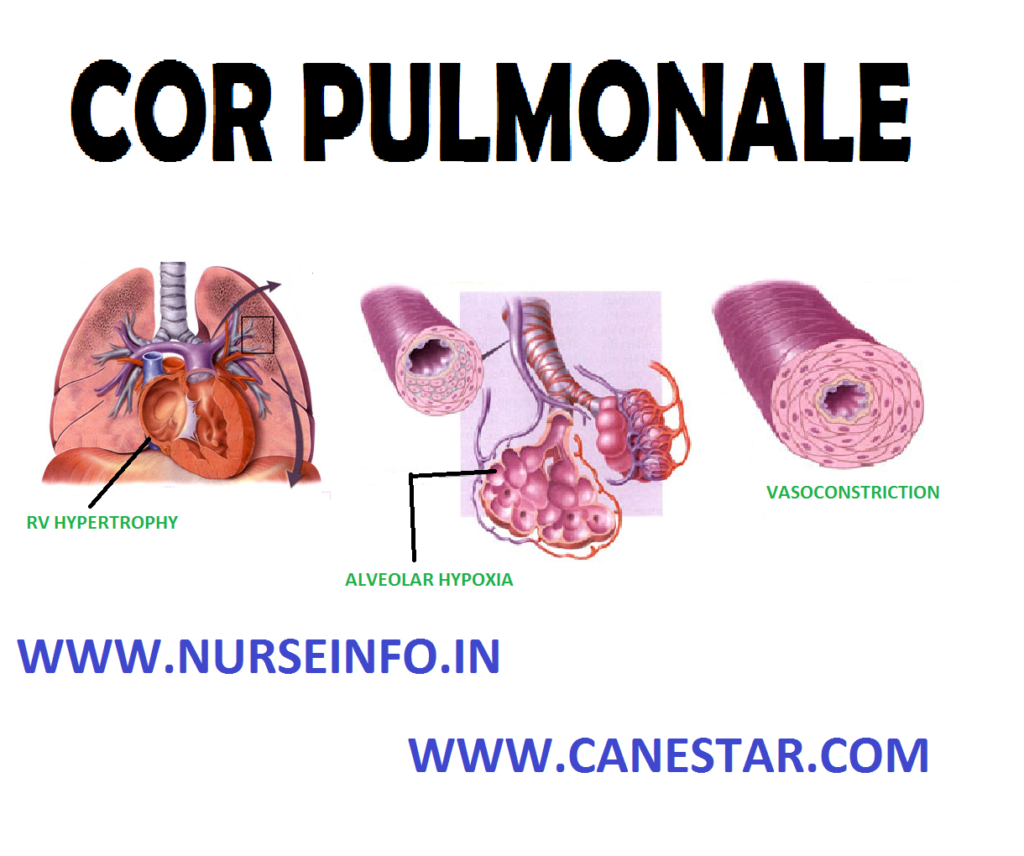
- Cor pulmonale refers to the altered structure (hypertrophy or dilatation) and impaired function of the right ventricle that results from pulmonary hypertension that is associated with diseases of the lungs (chronic obstructive pulmonary disease), vasculature (idiopathic pulmonary arterial hypertension), upper airway (obstructive sleep apnea), or chest wall (kyphoscoliosis).
ETIOLOGY
- Blood clots in the lungs
- COPD (chronic obstructive pulmonary disease)
- Lung tissue damages
- Sleep apnea
- Cystic fibrosis
- CHF
CLINICAL MANIFESTATIONS
Common symptoms that may suggest the presence of cor pulmonale in a patient with pulmonary or cardiopulmonary disease include:
- Worsening tachypnea (particularly at rest)
- Fatigue and lassitude
- Ankle swelling
- Worsening exertional dyspnea
- Worsening cough
- Angina-type chest discomfort
- Hemoptysis
- Hoarseness
- Late-stage hepatic congestion can cause symptoms (anorexia, jaundice and right upper quadrant abdominal discomfort)
- Cyanosis and plethora
- Chest markedly hyperexpanded
- Labored respiratory effort
- Intercostals recession
- Decreased air entry, crackles and wheeze in the chest
- Systolic bruits over lung fields
- Left parasternal or subxiphoid heave (a sign of right ventricular hypertrophy)
- Distended neck veins with raised and prominent JVP
- 3rd/4th heart sounds and pansystolic murmur of tricuspid regurgitation over right heart
- Split second heart sound with loud pulmonary component
- Systolic ejection murmur with a sharp ejection click over the pulmonary artery
- Diastolic pulmonary regurgitation murmur over the pulmonary artery
- Marked hepatojugular reflux due to hepatic congestion
- Hepatomegaly
- Jaundice in advanced cases
- Ascites in advanced cases
DIAGNOSTIC EVALUATION
The following investigations are often used to delineate the cause of respiratory compromise that may lead to cor pulmonale and to inform optimal management:
- Alpha-1 antitrypsin levels, if considered relevant
- Autoantibody screen if there is suspected collagen vascular disease
- Thrombophilia screen if there is suspected chronic venous thromboembolism
- Spirometry or lung function tests including gas transfer and flow volume loop
- CT and MRI scan of the chest
- Bronchoscopy
- Lung biopsy (open or transbronchial)
- Ventilation/perfusion scan/spiral-CT angiography/MRI-angiography
MANAGEMENT
- Long-term oxygen therapy or nocturnal oxygen therapy (NOT): it has been shown to improve quality of life and survival in patients with severe chronic hypoxia due to lung disease, by reducing pulmonary arteriolar constriction and improving and slowing the progression of cor pulmonale. They are usually recommended where PaCO2 is < 55 mm Hg or SaO2 is < 88%
- Diuretics: such as furosemide and bumetanide are frequently utilized, particularly where the right ventricular filling volume is markedly elevated, and in the management of associated peripheral oedema. Care must be taken to avoid overdiuresis which can impair the functioning of both the ventricles. It may also induce a hypokalemic metabolic alkalosis which can lessen respiratory drive through reducing the hypercapnea stimulus in breathe. Intravenous diuretics may be needed in patients with acute decompression and severe peripheral edema, due to poor absorption of oral medication
- Vasodilators: such as nifedipine and diltiazen can also be used to prevent chest pain
- Inotropic drugs, particularly digoxin, are frequently used to increase the cardiac output.
- Methylxanthine bronchodilators: such as theophylline are frequently used for their beneficial effect on bronchial tone
- Anticoagulation: it is used where patients have venous thromboembolism as the underlying cause of their cor pulmonale
- Venesection: it is used with caution is some patients who have severe secondary polycythemia due to chronic hypoxia
- Transplantation of lung and heart
COMPLICATIONS
- Exertional syncope
- Hypoxia and significantly limited exercise tolerance
- Peripheral edema
- Peripheral venous insufficiency
- Tricuspid regurgitation
- Hepatic congestion and cardiac cirrhosis
- Death
NURSING MANAGEMENT
Nursing Assessment
The nurse should assess the client for the clinical manifestations of CHF, especially in high-risk clients
- Impaired gas exchange related to fluid in the alveoli:
Auscultation of breath sounds every 4 hours
Encourage to turn cough and deep breath
Maintain Fowler’s position
Administer oxygen
Monitor ABG
Intubation and mechanical ventilation
- Decreased cardiac output related to heart failure and dysrhythmias
Vital signs every hour
Lung and heart sounds every 2 hours
Administer oxygen
Hourly urine output
Assess changes in mental status
Small meals
- Fluid volume excess related to reduced cardiac output and Na and water retention:
IO chart
Fowler’s position
Frequent oral care
Daily weighing
Assess jugular vein distension, peripheral edema, and hepatic engorgement
Fluid restriction
2-4 g salt diet
- Decreased peripheral tissue perfusion related to reduced cardiac output:
Monitor peripheral pulses
Color and temperature of skin
Keep extremities warm
Assess for thrombophlebitis
Active or passive ROM
- High risk for impaired skin integrity related to reduced peripheral tissue perfusions
Change position every 2 hours
Pressure mattress
Heel protectors
- High risk for digitalis toxicity related to impaired excretion:
Assess for hypokalemia, heart block
Serum digitalis levels and potassium