Asepsis in hospitals refers to the set of practices and techniques employed to prevent the introduction, growth, and spread of pathogenic microorganisms in the healthcare environment. The primary goal of aseptic techniques is to create and maintain a sterile or germ-free environment, reducing the risk of healthcare-associated infections (HAIs). Asepsis is critical in various healthcare settings, including operating rooms, patient care areas, and laboratories. Here are key components of asepsis in hospitals:
1. Hand Hygiene:
- Proper Handwashing: Healthcare workers must perform thorough handwashing with soap and water or use alcohol-based hand sanitizers before and after patient contact, after handling potentially contaminated materials, and between different procedures.
2. Personal Protective Equipment (PPE):
- Gloves, Masks, Gowns, and Eye Protection: Healthcare workers use appropriate PPE to protect themselves and patients from the transfer of microorganisms. The selection and proper use of PPE depend on the nature of the task and potential exposure.
3. Aseptic Techniques in Procedures:
- Sterile Techniques: During invasive procedures, surgeries, and certain medical treatments, sterile techniques are employed. This includes using sterile instruments, drapes, and dressings to prevent the introduction of microorganisms into sterile areas.
4. Environmental Cleaning and Disinfection:
- Regular Cleaning: Surfaces, equipment, and patient care areas are regularly cleaned to remove dirt and potential pathogens.
- Disinfection: Disinfectants are used to kill or inhibit the growth of microorganisms on surfaces. High-touch surfaces and medical equipment are prioritized for disinfection.
5. Sterilization:
- Autoclaving: Instruments and equipment that come into contact with sterile areas of the body or bloodstream are sterilized using autoclaves, ensuring the destruction of all microorganisms, including spores.
6. Isolation Precautions:
- Contact, Droplet, and Airborne Precautions: Patients with known or suspected infections are placed under appropriate isolation precautions to prevent the spread of pathogens.
7. Patient Placement and Room Design:
- Single-Patient Rooms: Hospitals may use single-patient rooms to minimize the risk of cross infection.
- Ventilation: Adequate ventilation and air filtration systems are crucial in preventing airborne transmission of pathogens.
8. Hand Antisepsis before Invasive Procedures:
- Pre-procedure Hand Antisepsis: Healthcare workers perform hand antisepsis using antiseptic solutions before engaging in invasive procedures to minimize the risk of introducing microorganisms.
9. Aseptic Technique in Intravenous (IV) Therapy:
- Sterile IV Procedures: Ensuring the use of aseptic technique when inserting and maintaining intravenous lines to prevent bloodstream infections.
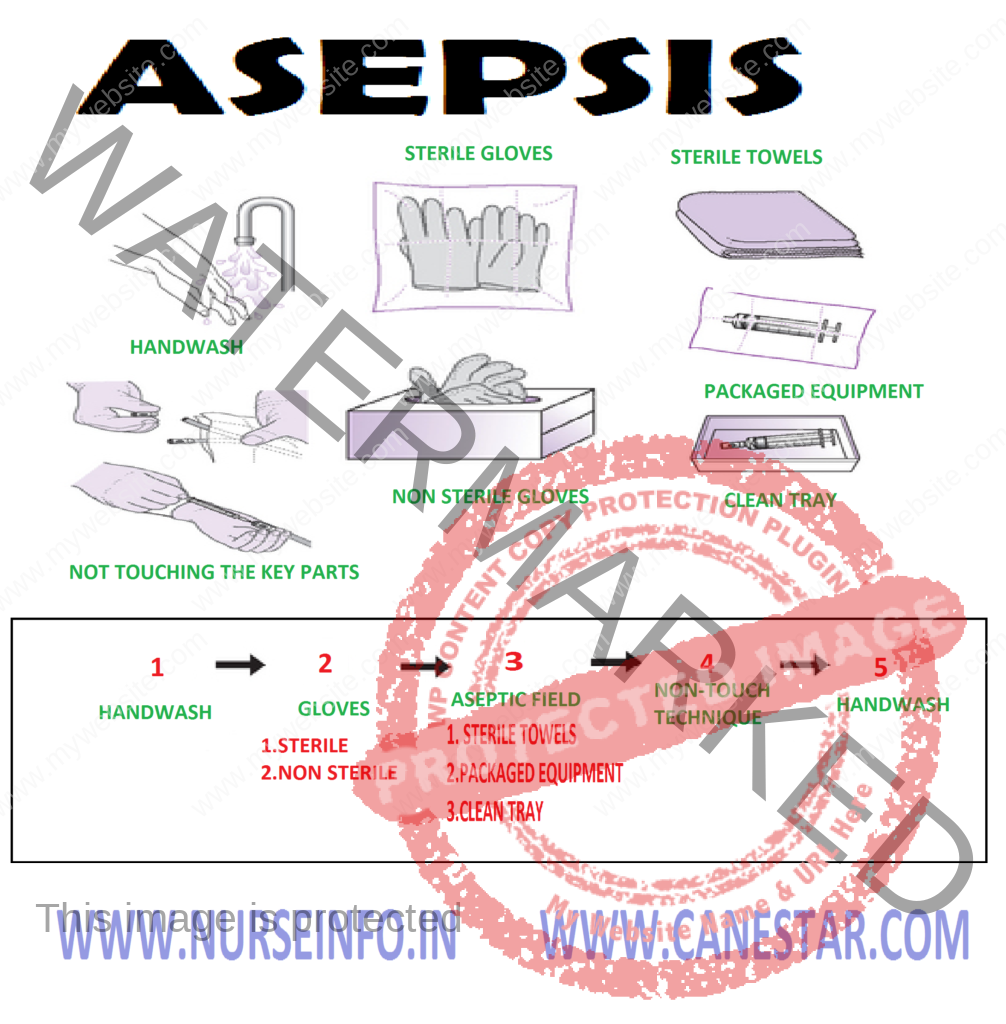
ASEPSIS
The practice of asepsis is designed to reduce the number of microorganisms present or reduce the risk of transmission from one person to another. It is also known as clean technique
Medical asepsis is the term used to describe the technique of preventing the transfer of disease by stopping the infection at its source or by reducing the number of pathogenic microorganisms after they have left the source
Medical Aseptic Technique Used to Break the Chain of Infection
- Daily change of patient bed linen
- Hand washing before and after each procedure
- Infected patients are separated from the non-infected patients (isolation of the patient)
- Hospital should be well ventilated
- Maintenance of general cleanliness of the hospital
- Safe food and water, water chlorination
- Safe disposal of excreta and refuse
- Destruction of rodents and insects
- Disinfection and sterilization of supplies
- Immunization – it is the act of creating immunity artificially against a particular disease
- Maintenance of personal hygiene of the patient
- Use of mask, gown and gloves in needed cases
- Keeping toilet articles separate for each person
- Minimizing the number of visitors
- Health education to the patient and relatives
METHODS/TYPES OF ISOLATION
Strict isolation: it prevents spread by contact in case of rabies, tetanus, anthrax, scabies, leprosy and venereal diseases, nurses must wash hands frequently and thoroughly use disposable supplies and discard them properly. Send reusable supplies for disinfection and sterilization. Wear gown, mask and gloves
Respiratory isolation: it is indicated in situations where the pathogens are spread on droplets from the respiratory tract. In this type of infection nurses should wear mask and gown while caring for the patient. Use articles should be disinfected avoid the possibility of contamination. Handkerchiefs should be cleaned and disinfected before reuse. Maintain reasonable distance to prevent droplet infection, the diseases are whooping cough, influenza, diphtheria, measles, etc
Enteric isolation: it is indicated when the pathogens are transmitted in feces, for this type isolation, it is not necessary to wear a mask, but it is recommended that gloves and gowns be worn when handling soiled articles. Thorough hand washing should be emphasized both by the patients and nurses. The excreta may be disinfected by adding lime before its disposal. The soiled articles such as linen should be disinfected before sending to laundry
Wound and skin isolation: this type of isolation is for pathogens which are found in wound and can be transmitted by the contact with the wounds. Usually gowns and gloves are worn in this type of infection. Important point to remember is the safe disposal of dressing and discharges from the wounds and disinfection of articles. Strict isolation techniques should be followed when caring for patients with abscesses, boils, infected burns, gag gangrene, anthrax, rabies, etc. all the articles used for these patients should be kept separated
Great care should be taken by the nurses to prevent cuts or abrasions on their hands, frequent and thorough hand washing reduces the chance of infection
Blood isolation: this type of isolation is intended to prevent transmission of pathogens that are found in the blood. Therefore, any equipment that comes in contact with the patient’s blood should be carefully disinfected before touching another object or person. Use of mosquito nets also emphasized to prevent this type of infection.
Following Precautions to be Taken While Caring for Infectious patients
- Yearly physical examination including chest X-ray
- Well balanced diet
- Proper hand washing after elimination, before eating, before and after every procedure
- Proper immunization
- Children below 12 years should not be allowed in to the ward
- As far as possible maintain two bed to avoid cross infection
- Restrict visitors
- Proper health education to patient, visitor and relatives
Principle of Surgical Asepsis
Principles
- Always face the sterile field. Do not turn back or side on a sterile field
Rationale: Sterile objects which are out of vision are considered questionable and their sterility cannot be guaranteed
- Keep sterile equipment above your waist level or above table level
Rationale: Waist level and table level are considered margins of safety and will promote maximum visibility of the sterile field
- Do not speak, sneeze and cough over a sterile field
Rationale: To prevent droplet infection
- Never reach across sterile field
Rationale: when a non-sterile object is held above a sterile object, gravity causes microorganisms to fall into the sterile field
Types of Asepsis
Surgical asepsis: refers to procedures used to keep objects of areas sterile or completely free from all microorganisms. The techniques are used in the operating room and in some treatments where aseptic technique is to be followed
Medical asepsis: refers to all procedures used to protect the patient and his environment from the transmission of diseases producing organisms that can transmit from one patient to another. This involves strict sterilization of some articles and methods to maintain cleanliness of others. Correct hand washing is very important in carrying out medical asepsis
Types of Aseptic Practices
- Cleaning: it includes dusting, sweeping and moping the unit, rinsing and washing the equipment and patient to remove pathogens
- Hand washing: cleaning hands to remove pathogens
- Capping and masking: capping is covering the head and masking is covering the nose and mouth to protect the nurse from inhaling pathogens when disease is air borne
- Gowning: it means covering the uniform to protect the nurse from contaminating herself and others around her
- Gloving: it means covering the hands to protect the nurse or patient with poor resistance from pathogens
- Bagging: it means removing the contaminated materials and supplies in bags from isolation unit
DIFFERENCE BETWEEN MEDICAL AND SURGICAL ASEPSIS
Medical Asepsis
- A clean technique is used
- Transmission of pathogenic organisms is prevented, e.g. hair combing, mouthwash
- Patient and his environment is protected from cross infection
Surgical Asepsis
- Sterile technique is used
- Pathogenic and non-pathogenic organisms are totally prevented, e.g. giving injections, dressing
- Objects or articles are free from pathogenic and non-pathogenic pathogenic organisms