ARTIFICIAL AIRWAY MANAGEMENT – Definition, Indications, Endotracheal Route of Insertion, Tube Types, General Instructions, Equipment, Preparation of the Patient and the Environment, Procedure, After Care and Complications
DEFINITION
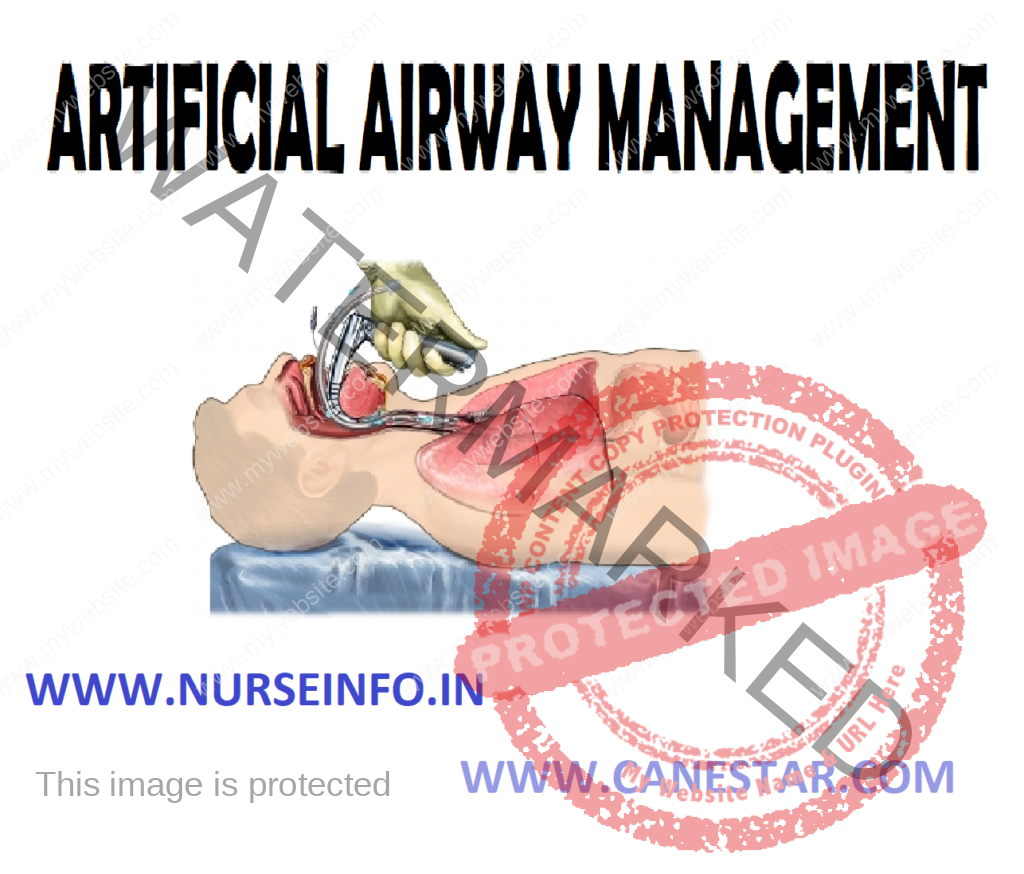
An artificial airway is a tube that is inserted at the mouth or nose or level of the second or third tracheal ring to permit mechanical ventilation and facilitate secretion removal. The distal end of the tube is located in the trachea below the vocal cords.
INDICATIONS
- Acute respiratory failure, central nervous system (CNS) depression, neuromuscular disease, pulmonary disease, chest wall injury
- Upper airway obstruction
- Anticipated upper airway obstruction from edema or soft tissue swelling due to head and neck trauma, some postoperative head and neck procedures involving the airway facial or airway burns, decreased level of consciousness
- Aspiration prophylaxis
- Fractured cervical vertebrae with spinal cord injury requiring ventilator assistance
ENDOTRACHEAL ROUTE OF INSERTION
Tube can be inserted through nose or mouth. A cuff is always located at the distal end of the tube.
- Orotracheal: insertion of an oral tube is technically easier, since it is done under direct visualization. Disadvantages are increased oral secretions, decreased patient comfort, difficulty with stabilization, and inability of the patient to use lip movement as a communication.
- Nasotracheal: may be more comfortable to the patient and is easier to stabilize. Disadvantages are that blind insertion is required, possible development of pressure necrosis of the nasal airway, sinusitis and otitis media
TUBE TYPES
- Vary according to length and inner diameter in millimeters
- Vary according to cuff, most are high volume, low pressure with self-sealing inflation valves or the cuff may be foam rubber (foam cuff)
- Vary according to composition and cuff type synthetic Teflon, nylon, polyvinyl chloride, polyethylene or silastic. May or may not have inner cannula. Usually are cuffed.
- Tubes with high volume, low pressure cuff self-sealing inflation valves and with or without inner cannula
Pressure limiting cuffs
Polyurethane foam filled cuffs
Speaking tracheotomy tube
Fenestrated
- Usual sizes for adult are 6.0, 7.0, 8.0, and 9.0 mm
GENERAL INSTRUCTIONS
Physical Management
- Ensure adequate ventilation and oxygenation through the use of mechanical ventilation, continuous positive airway pressure (CPAP) device, Briggs T-piece adapter
- Provide adequate humidity, since the natural humidifying pathway of the oropharynx is bypassed. Clear airway of secretions as needed with suctioning
- Use aseptic technique when entering the artificial airway. The artificial airway is sterile below the level of the vocal cords
- Frequently assess the patient’s need for ventilator assistance
- Elevate the patient to a semi-Fowler’s or sitting position, when possible, since these positions resulting improved lung compliance. The patient’s position however, should be changed at least every 2 hours, to ensure ventilation of all lung segments and prevention of secretion stagnation. Position changes are also necessary to avoid skin breakdown
- Nutrition endotube: recognizes that the tube holds open the epiglottis. Therefore, only the inflated cuff prevents the aspiration of oropharyngeal contents into the lungs. The patient must not receive oral feeding. Nutrition must take the form of external tube feedings.
- Be aware of the complications and damage that inflated cuffs may have on the tracheal mucosa. Endotracheal tube cuffs should be inflated continuously and deflated only during intubations, extubations, and tube repositioning. The internal cuff pressure should be checked every 2 hours
- External tube site care endotube: patients with endotracheal tubes have mouth care every shift, or a frequently as needed. Oral secretions tend to stagnate and risk oral infection is increased. An oral endotracheal tube may also stimulate an increase in the production of oral secretions. The tube must be secured at all times and the ventilator, CPAP or T-piece tubing supported so that traction is not applied to the tube
- Have available at all times all the patient’s bedside a resuscitation bag, oxygen bag source and mask to ventilate the patient in the event of accidental removal anticipate your course of action in such an event
- Endotracheal tube: know the location and assembly of reintubation equipment. Know the method of contact personnel capable of reintubation
PSYCHOLOGICAL CARE OF THE PATIENT
- Recognize that the patient is usually apprehensive particularly about choking inability to communicate verbally, being unable to remove secretions, difficulty in breathing, or mechanical failure
- Explain the function of the equipment carefully
- Inform the patient and his family that he will not be able to speak while the tube is in place being a tracheostomy tube
EQUIPMENT
- Laryngoscope with curved or straight blade and working light source
- Endotracheal tube with low pressure cuff and adapter to connect tube to ventilator or resuscitation bag
- Stylet to guide the endotracheal tube
- Oral airway or bite block to keep the patient from biting into and occluding the endotracheal tube
- Adhesive tape or tube fixation system
- Sterile anesthetic lubricant jelly
- Syringe
- Suction source
- Suction catheter and tonsil suction
- Resuscitation bag and mask connected to oxygen source
- Anesthetic spray
PREPARATION OF THE PATIENT AND THE ENVIRONMENT
- Suction endotracheal tube
- Suction oropharyngeal airway above the endotracheal cuff as thoroughly as possible
- Loosen tape or endotracheal tube securing device
- Extubate the patient
Ask the patient to take as deep as a breath as possible
At peak inspiration deflate the cuff completely and pull the tube out in the direction of the curve
- Once the tube is fully removed, ask the patient to cough or exhale forcefully to remove secretions. Then suction the back of the patient’s airway with the tonsil suction
- Evaluate immediately for any signs of airway obstruction, stridor or difficult breathing. If the patient develops any of the above problems, attempt to ventilate the patient with the resuscitation bag and mask and prepare for reintubation
- Administer oxygen as directed
AFTER CARE
- Observe patient closely post-extubation for any signs and symptoms of airway obstruction or respiratory insufficiency
- Observe character of voice
COMPLICATIONS
Mechanical
- Cuff leaks
- Cuff herniation
- Tube obstruction
- Tube displacement
- Inadvertent extubation
- Right main stem intubation
Laryngeal and Tracheal
- Sore throat
- Hoarse voice
- Glottic edema
- Ulceration of tracheal mucosa
- Vocal cord ulceration, granuloma, or polyps
- Vocal cord paralysis
- Laryngotracheal web: formation of a web fibrin and cellular debris initiated by neuro tissue at the glottic or subglottic level
- Post-extubation tracheal stenosis
- Formation of tracheoesophageal fistula