COAL WORKER’S PNEUMOCONIOSIS – Causes, Pathophysiology, Signs and Symptoms, Diagnostic Evaluation and Management
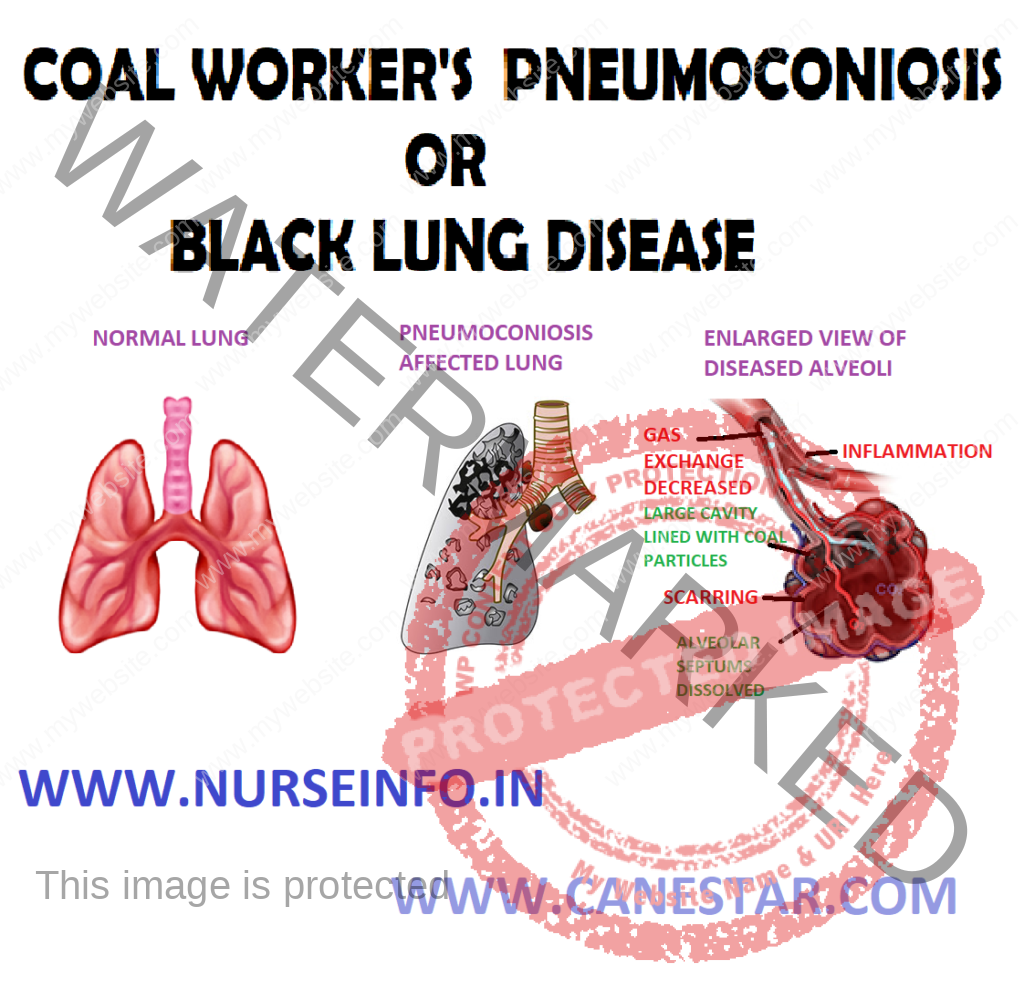
- Coal worker’s pneumoconiosis (CWP) can be defined as the accumulation of coal dust in the lungs and the tissue’s reaction to its presence
- Pneumoconiosis, also known as Black Lung Disease, is an occupational lung disease caused by inhaling coal dust. There are two types of pneumoconiosis – simple, known as coal worker’s pneumoconiosis (CWP) and complicated, known as progressive massive fibrosis (PMF)
CAUSES
- Type of dust: more silica increases the risk of fibrosis. Coal rankings are as follows:
High: this coal is older and has the least amount of volatile matter (e.g. anthracite coal)
Medium: this coal is of moderate age and has a greater amount of volatile matter (e.g. bituminous coal)
Low: this coal is younger and has the greatest amount of volatile matter (e.g. lignite coal)
- Age at first exposure
- Length of time spent underground
- Smoking
- Size of dust particles
- Type of job: certain job requires more exposure to dust. Most dust is found at the coal face; therefore, individuals who work directly on the cutting of the coal have the highest exposure. The following list details dust exposure related to job title, beginning with the highest exposure:
Cutting-machine operator: this worker cut coal directly at the face. Respirable dust levels are highest here
Roof bolters: these individuals drill through rock and thus also exposed to silica. The continuous mine operator, loading machine operator, and shot firer are also exposed to higher amounts of respirable dust
Train operators: they drop sand onto the tracks for traction and may, therefore, develop silicosis
Motormen, brakemen, drivers and shuttle care operators: these individuals have less dust exposure because the coal has already been cut by the time they work with it, thus decreasing their exposure to respirable dust.
Mechanics, electricians and maintenance personnel: they have the least amount of dust exposure
PATHOPHYSIOLOGY
Coal dust that enters the lungs can neither be destroyed nor removed by the body —- the particles are engulfed by resident alveolar or interstitial macrophages —- remain in the lungs, residing in the connective tissue or pulmonary lymph nodes —- coal dust provides a sufficient stimulus for the macrophages to release various products, including enzymes, cytokines, oxygen radicals, and fibroblast growth factors —- aggregations of carbon-laden macrophages can be visualized under a microscope as granular, black areas. In serious cases, the lung may grossly appear black —- these aggregations can cause inflammation and fibrosis, as well as the formation of nodular lesions within the lungs —- the centers of dense lesions may become necrotic due to ischemia, leading to large cavities within the lung
SIGNS AND SYMPTOMS
- First stage is called simple pneumoconiosis, which is characterized by chronic cough, fever, expectoration and dyspnea on exertion. This is associated with little ventilator impairment. This stage will develop after 10-12 years of exposure
- Second stage is called progressive massive fibrosis: it is irreversible and continues even after cessation of the exposure. Prognosis is not good.
DIAGNOSTIC EVALUATION
- History of exposure
- Lung function test: varies from normal to obstructive or restrictive or combination of both. Diffusion decreased. Dyspnea on exertion. X-ray chest: small nodules, 1-10 mm in upper lung zones, and ground glass appearance of the lung
- Radiograph of CWP
- Pulmonary function tests: used to test the ability of the lungs to take in air (inspiration). Often used in conjunction with the X-ray chest. Forced vital capacity (FVC) and FEV1 (forced expiratory volume in one second) are used to diagnose lung disease
MANAGEMENT
Corticosteroids, pulmonary lavage, lung transplant
Prevention and Control
- Preplacement and periodic medical examination of workers
- Use of protective equipment by the workers
- Use of dust suppression measure
- Gravimetric dust sampling in dusty areas
- Exhaust ventilation
COMPLICATIONS
- Respiratory: pneumothorax, chronic obstructive pulmonary disease, cor pulmonale
- Infectious diseases: tuberculosis, vascular diseases
NURSING MANAGEMENT
Nursing Diagnosis
- Impaired gas exchange related to cough and pain from incision:
- Open the airway with headtilt, chinlift, jaw thrust
- Set the position to maximize ventilation
- Use tools airway
- Perform chest physiotherapy
- Teach breathing deeply and coughing effectively
- Perform suction
- Auscultation of breath sounds
- Give bronchodilators (collaboration)
Oxygenation therapy
- Provide humidification system of oxygen equipment
- Monitor the flow of oxygen and the amount given
- Monitor signs of oxygen toxicity
- Risk for hemorrhage related to transplant procedure:
- Monitor pulse rate
- Monitor central venous pressure
- Provide sterile dressing on wound
- Give vitamin K as per doctor’s advice
- Pain related to surgical condition as evidenced by verbal communication
- Assess for the presence of pain, the scale, and intensity of pain
- Teach the client about pain management and relaxation with distraction
- Secure the chest tube to restrict movement and avoid irritation
- Assess pain-reduction measures
- Provide analgesics as indicated