THORACENTESIS – Definition, Purpose, General Instructions, Preliminary Assessment, preparation of the Patient and Environment, Equipment, Procedure, After Care and Complications
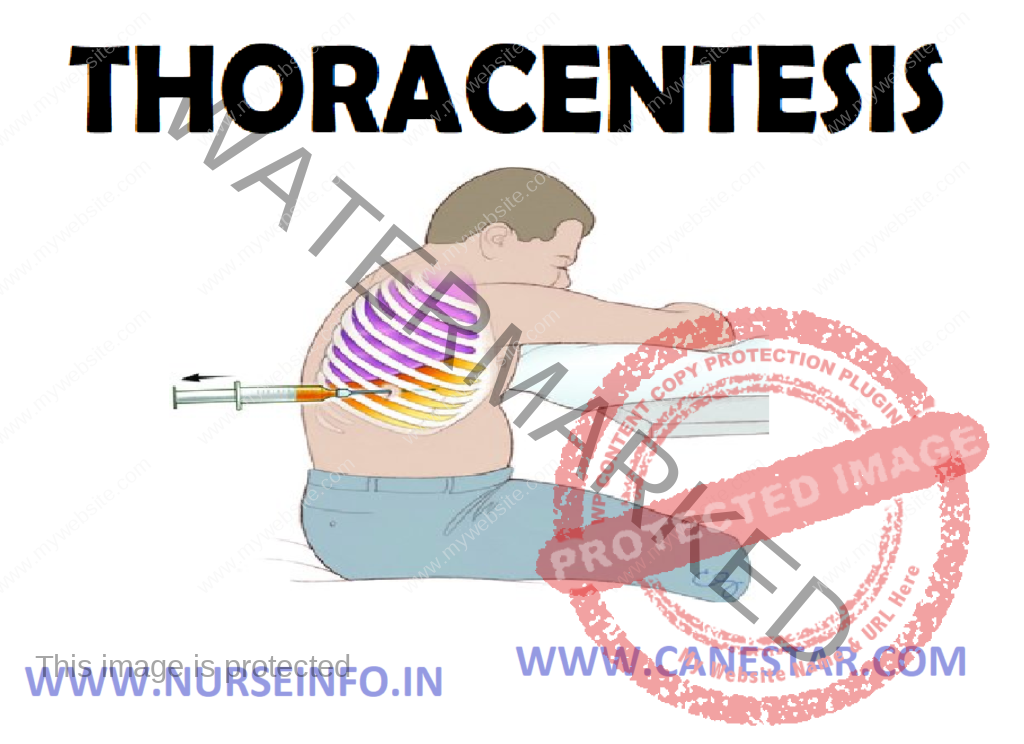
Thoracentesis is defined as introducing a hollow needle into pleural cavity and aspirating fluid or air, using aseptic technique.
Thoracentesis refer to the puncture by needle through the chest wall into the pleural space for the purpose of removing pleural fluid (blood, serous fluid, pus, etc) and or air (pneumothorax)
Thoracentesis or pleural aspiration or pleural tap is the insertion of needle into the pleural space through the chest wall to remove the pleural fluid or possibly air
DEFINITION
A thoracentesis is a surgical puncture of the chest wall to aspirate fluid or air from the pleural cavity. A pleural effusion is an abnormal accumulation of fluid in the pleural space.
PURPOSE
- To remove excessive pleural fluid (serous fluid, blood or pus)
- To drain fluid/air from pleural cavity for diagnostic or therapeutic purposes
- To introduce medications
- To aid in full expansion of lung
- To obtain specimen for biopsy
- To take pleural biopsy for diagnostic examination
- To relieve pain
- To relieve breathlessness caused by accumulation of fluid or air in the pleural space
- To aid in diagnosis and treatment (chemical, bacteriological, cellular, composition and malignancy)
GENERAL INSTRUCTIONS
- The patient should be prepared physically and psychologically for the procedure
- Thoracentesis is indicated in case of pleural effusion due to infection, traumatic injury, cancer or cardiac diseases, etc
- Common site for thoracentesis is just below the scapula at the seventh or eighth intercostals space
- The patient should be warned that any sudden movements during the procedure may cause injury to the lungs, blood vessels, etc
- The level of the aspiration needle should be short to prevent pricking of the lungs
- Usually upright position is used during the procedure as it helps collect the pleural fluid at the base of the pleural cavity and hence facilitates to remove the fluid easily
- Maintain strict aseptic technique to prevent introduction of infection into the pleural space
- The 3 way adaptor should be fitted with the needle before it is introduced into the chest cavity. The adaptor should be in a closed position to prevent the entry of air into the pleural cavity
- The nurse should check the syringes and needle for air-tightness. If these are not air-tight, air may be entering the pleural cavity and collapse
- Remove the fluid slowly and not more than 1000 ml at the time, if the tap is therapeutic to prevent mediastinal shift
- Use water: seal drainage system, if pleural fluid is purulent and difficult to drain
- The specimen should be sent to the laboratory soon after it collected
- The aspiration should be discontinued if any signs of complications are noted such as sharp pain, respiratory distress, excessive coughing, crepitus, haemoptysis, circulatory collapse, etc
PRELIMINARY ASSESSMENT
Check
- Doctors order for any specific instructions
- Written informed consent of the patient or relative
- General condition and diagnosis of the patient
- Review fresh erect chest X-ray
- Confirm the diagnosis, location and extent of the pleural air/fluid/pus
- Acute respiratory insufficiency (tension pneumothorax, rapidly developing effusion without dyspnea) may demand thoracentesis without X-ray
- Mental status of the patient to follow instructions
- Articles available in the unit
PREPARATION OF THE PATIENT AND ENVIRONMENT
- Explain the sequence of the procedure
- Provide privacy
- Chest X-ray should be taken before thoracentesis is done to diagnose the location
- Check the vital signs and record it on the nurse’s record for reference
- A mild sedation may be given to the patient before starting the procedure
- Maintain the desired position during the procedure
- The nurse should remain near the patient to observe him and to remind him not to move during the procedure
- Arrange the articles at the bedside or in the treatment room
- Premedication – inj. Atropine sulfate 0.65 mg intramuscularly or intravenously half an hour before procedure
EQUIPMENT
A sterile tray containing:
- Sponge holding forceps – 1
- Dissecting forceps – 1
- Syringe (5 ml) and 2 needles for giving local anesthesia
- 20 ml syringe with 1 leur lock to aspirate the fluid
- Aspiration needle No. 16 (long and short)
- 3 way stopcock
- Small bowls – 2 to take the cleaning lotions
- Specimen bottles and slides
- Cotton swabs, gauze pieces and cotton pads
- Gown, masks and gloves for the doctor
- Sterile dressing towels/slit
An unsterile/clean tray containing:
- Mackintosh and towel
- Kidney tray and paper bag
- Spirit, iodine, tincture benzoin
- Lignocaine 2%
- Suction apparatus with water seal drainage system
PROCEDURE
- Position the patient in Fowler’s. bring patient to one side of bed with feet supported, arms and head leaning forward on cardiac table with pillows
- Unite gown to expose site for aspiration
- Instruct patient to avoid coughing and to remain immobile during procedure
- Explain that a feeling of deep pressure will be experienced while fluid is being aspirated from pleural space
- Provide sterile gloves to doctor
- Open sterile set and assemble 20 ml, 50 ml syringes, 20-22 G needles and aspiration needles
- Pour antiseptic solution to clean site
- After showing label to doctor clean top of local anesthetic bottle and assist to withdraw mediation
- Reassure patient and instruct to hold breath during insertion of aspiration needle
- As physician does procedure, observe for signs and symptoms of complications
- After fluid is withdrawn from pleural space, transfer to specimen container
- After needle is withdrawn, apply pressure over puncture site. Assist in sealing site with tincture benzoin swab
AFTER CARE
- Instruct patient to lie on on-affected site for 1 hour. Ensure bed rest for 6-8 hours
- Monitor vital signs every half hour until stable
- Observe patient for signs and symptoms of hemothorax, tension penumothorax, subcutaneous emphysema, and air embolism
- Administer analgesics and antibiotics as prescribed
- Instruct patient to carry out deep breathing exercises
- A chest X-ray may be taken to determine the effects of the procedure
- The puncture site should be treated aseptically to prevent contamination of the wound
- The container with aspirated fluid should be labeled and sent to the laboratory with requisition form
- Replace the articles after cleaning
- Wash hands thoroughly
- Record the procedure in the nurse’s record sheet
COMPLICATIONS
- Pneumothorax and hemothorax: sudden rise of sharp pain in the chest, persistent cough, shortness of breath, fall in blood pressure, rapid pulse, anxiety, restlessness, and faintness, profuse sweating, pallor and cyanosis
- Tension pneumothorax: marked dyspnea, cyanosis, reduced or absence of breath sounds and decreased movement of chest on respiration on the affected site. Acute chest pain, increased pulse and respiratory rates. Shifting of the trachea to the unaffected side
- Mediastinal shift: cyanosis, severe dyspnea, deviation of larynx and trachea from their normal midline position towards the unaffected side, shifting of the heart heat position of maximum impulse and distended neck veins
- Pulmonary edema: blood tinged frothy sputum
Cough, wheezing, severe dyspnea
Cyanosis, tachycardia, tachypnea, distended neck
Veins, signs of heart failure, peripheral edema
Altered level of consciousness


Very informative