SELECTION OF SITE FOR INJECTION
Selection depends upon the following:
- Route of administration ordered by doctor
- Quantity of the drugs
- Condition of the patient
- Muscular development
- Knowledge of anatomical position of the nerves
- Rotation of the site is necessary to avoid tissue trauma
Technical Skill Needed
- Arrange the required equipment for the procedure
- Nurse must be very skillful while giving the injection according to the route ordered
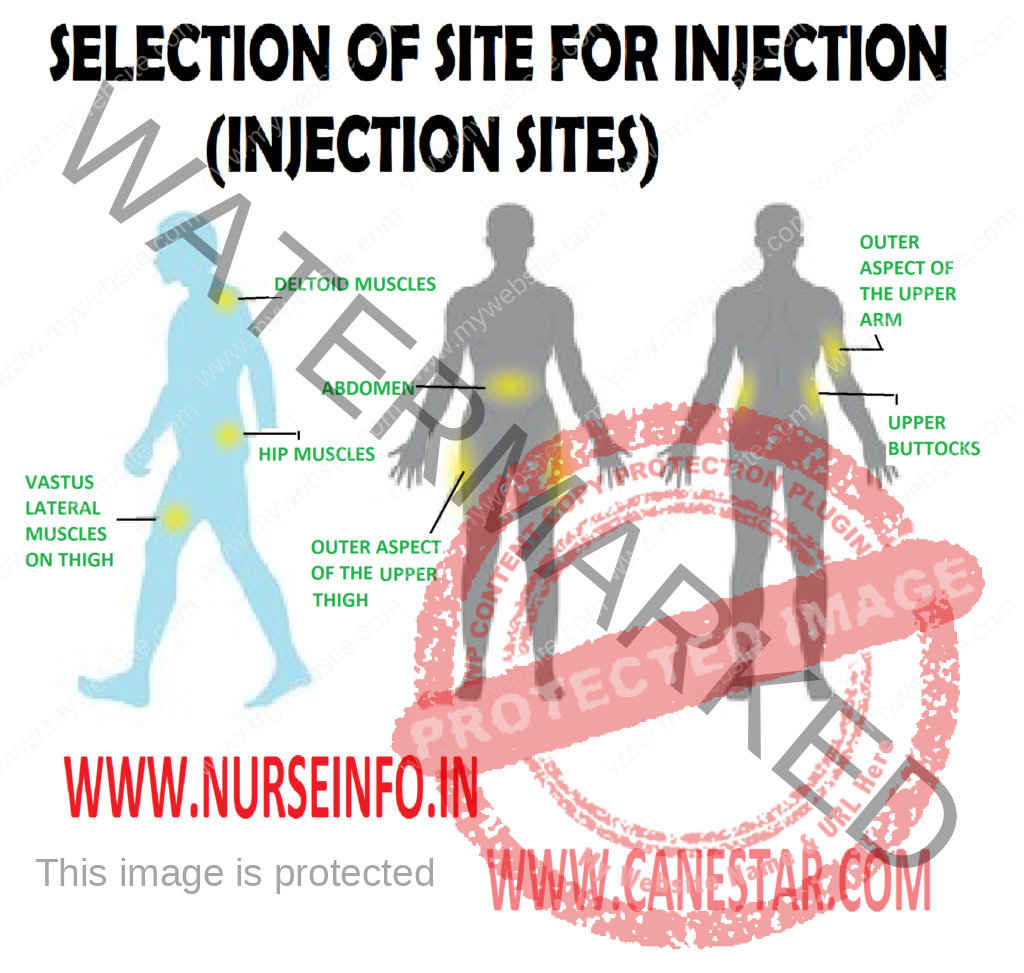
- Select correct site for injection
- Prepare the medication dose accurately
Criteria for Selection of Syringes and Needles
- Intradermal: tuberculin syringe or 1 ml calibrated in 0.01 ml units. 26 or 27 gauge diameter and 3/8 to 5/8 length size of needle used
- Subcutaneous: insulin syringe or 1 ml calibrated in 40 or 80 unites syringe. 25 gauge and ½ to 5/8 inches syringe is used
- Intramuscular: 2.5 ml syringe is used it calibrated in 0.2 ml. 21, 22, 23 gauge 1 to 2 inches in length needles are used
- Intravenous: the size depends upon the amount of fluids to be injected, 18 to 20 gauge 1 to 2 inches needles use
Golden Rules of Giving Injections
Administer the right drug: to prevent mistakes, take time to check the name and spelling of each drug you administer against the patient’s medicine card. Check a drug, at least, twice before giving it. First, when you remove it from the stock cupboard and, second time, before administering it to the patient. Avoid distractions. If you are unfamiliar with the ordered drug, learn about the drug from the pharmacist and the doctor. When in doubt, clear the doubt from the doctor.
Administer the drug to the right patient: make sure that the name of the patient is correct before you give the medicines. Check the name, diagnosis, and IP number. Adopt as a practice to confirm the right patient each time you administer the drug. Never leave a drug at the patient’s bedside
Administer the right dose: you must check and double check the drug dose ordered against the dose you are about to give. Be especially careful when you are administering toxic medications, such as antineoplastic drugs. With these, the margin between a therapeutic and a potentially lethal dose is slim. Use an infusion as indicated and monitor the patient closely especially after an initial or loading dose is given or any time a close is increased
Administer the drug by the right route: the parenteral route demands more vigilance. Parenteral drugs act so rapidly that a medication error may be very harmful – even fatal. If the order doesn’t specify a route, call the doctor immediately for a clarification
Administer the drug at the right time: therapeutic blood levels of many drugs depend on consistent, regular administration times. Never give a drug more than half an hour before or after the scheduled time, without checking with the doctor
A hospital drug policy manual is one way to prevent errors associated with administration times. Make sure you coordinate drug administration with the laboratory schedule
Educate your patient about the drug he is receiving: take advantage of every opportunity to teach your patient and his family about his prescribed medication. Stress the need for consistent and timely administration. Make sure they understand the importance of taking the medications for the entire prescribed course. Many patients, who begin to feel better after the first few doses, stop taking the drug
Take patient’s complete drug history: it is necessary to know all the drugs your patient has been receiving and all the help he wants. By doing this you ensure his safety. The risk of adverse drug reactions and interactions, of course, rises with the member of drugs being taken
Find out if the patient has any drug allergies: no drug is completely safe. Any drug may cause an unpredictable reaction producing many different adverse effects – some appearing immediately, others developing over a period of time. Stay alert as you assess your patient’s reaction to any drug you give him. Warm him that he should avoid drugs that have caused even a mild allergic response
Be aware of potential drug/drug or drug/food interactions
Document each drug you administer: never document a drug before administering it but document you must after it is administered