PULMONARY HYPERTENSION – Introduction, Types, Etiology, Pathophysiology, Clinical Manifestations, Diagnostic Evaluations and Management
INTRODUCTION
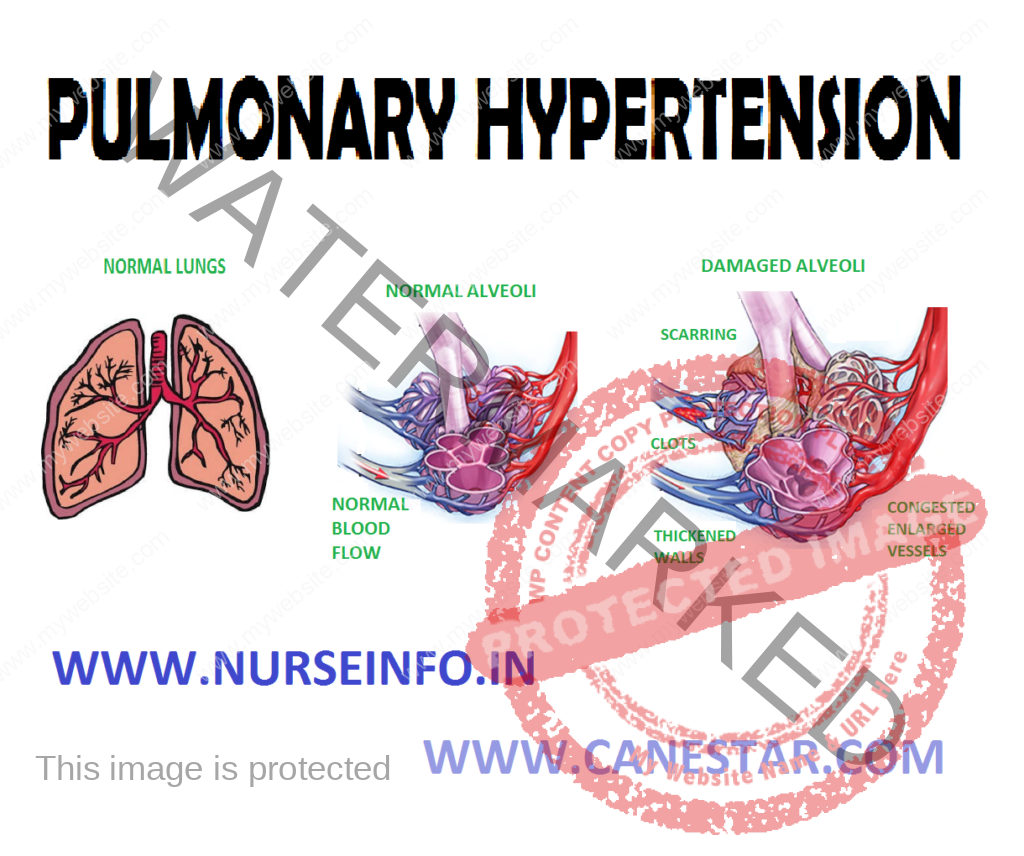
- Pulmonary hypertension (PH) is high blood pressure in the arteries to lungs. It is a serious condition. The blood vessels that carry blood from heart to lungs become hard and narrow. Heart has to work harder to pump the blood through. Over time, heart weakens and cannot do its job and can develop failure.
- Pulmonary hypertension (PH) is an increase of blood pressure in the pulmonary artery, pulmonary vein, or pulmonary capillaries, together known as the lung vasculature, leading to shortness of breath, dizziness, fainting, leg swelling and other symptoms.
TYPES OF PULMONARY HYPERTENSION
- Idiopathic Pulmonary Hypertension
When an underlying cause for high blood pressure in the lungs cannot be found, the condition is called idiopathic pulmonary hypertension (IPH). Some people with IPH may have a gene that is a risk factor for developing pulmonary hypertension. But in most people with idiopathic pulmonary hypertension, there is no recognized cause of their pulmonary hypertension.
- Secondary Pulmonary Hypertension
Pulmonary hypertension that is caused by another medical problem is called secondary pulmonary hypertension. This type of pulmonary hypertension is more common than idiopathic pulmonary hypertension. Causes of secondary pulmonary hypertension include:
- Blood clots in the lungs (pulmonary emboli)
- Chronic obstructive pulmonary diseases, such as emphysema
- Connective tissue disorders, such as scleroderma or lupus
- Sleep apnea and other sleep disorders
- Congenital heart disease
- Sickle cell anemia
- Chronic liver disease (cirrhosis)
- AIDS
- Lung diseases, such as pulmonary fibrosis
Other Types of Pulmonary Hypertension
The World Health Organization divides pulmonary hypertension (PH) into five groups. These groups are organized based on the cause of the condition and treatment options. In all groups, the average pressure in the pulmonary arteries is 25 mm Hg or higher. The pressure in normal pulmonary arteries is 8-20 mm Hg at rest.
Group 1 Pulmonary Arterial Hypertension
- PAH that has no known cause
- PAH that is inherited (passed from parents to children through genes)
- PAH that is caused by drugs or toxins, such as street drugs and certain diet medicines
- PAH that is caused by conditions such as:
Connective tissue diseases (connective tissue helps support all parts of your body, including your skin, eyes, and heart).
HIV infection
Liver disease
Congenital heart disease. This is heart disease that is present at birth
Sickle-cell disease
- PAH that is caused by conditions that affect the veins and small blood vessels of the lungs
Group 2 Pulmonary Hypertension
Group 2 includes PH with left heart disease. Conditions that affect the left side of the heart, such as mitral valve disease or long-term high blood pressure, can cause left heart disease and PH. Left heart disease is likely the most common cause of PH.
Group 2 Pulmonary Hypertension
Group 3 includes PH associated with lung diseases, such as COPD (chronic obstructive pulmonary disease) and interstitial lung diseases. Interstitial lung diseases cause scarring of the lung tissue. It is also associated with sleep-related breathing disorders, such as sleep apnea.
Group 4 Pulmonary Hypertension
Group 4 includes PH caused by blood clots in the lungs or blood-clotting disorders.
Group 5 Pulmonary Hypertension
Group 5 includes PH caused by various other diseases or conditions. Examples include:
- Blood disorders, such as polycythemia vera and essential thrombocythemia
- Systemic disorders, such as sarcoidosis and vasculitis
- Metabolic disorders, such as thyroid disease and glycogen storage disease
- Other conditions, such as tumors that press on the pulmonary arteries and kidney disease
ETIOLOGY
- Drugs: for example, dexfenfluramine and phentermine have been taken off the market. It increases risk of developing pulmonary hypertension
- Liver diseases, rheumatic disorders, lung conditions: pulmonary hypertension can also occur as a result of other medical conditions, such as chronic liver disease and liver cirrhosis, rheumatic disorders, such as scleroderma or systemic lupus erythematosus (lupus) and lung conditions including tumors, emphysema, chronic obstructive pulmonary disease (COPD), and pulmonary fibrosis
- Certain heart diseases: heart diseases including aortic valve disease, left heart failure, mitral valve disease, and congenital heart disease can also cause pulmonary hypertension
- Thromboembolic disease: a blood clot in a large pulmonary artery can result in the development of pulmonary hypertension
- Low-oxygen conditions: high-altitude living, obesity, and sleep apnea can also lead to the development of pulmonary hypertension
- Genetic predisposition: pulmonary hypertension is inherited in a small number of cases. Knowing that someone in the family has or has pulmonary hypertension should prompt you to seek early evaluation should symptoms occur.
- Pulmonary hypertension may also be caused by other conditions, and in some cases, the cause is unknown
PATHOPHYSIOLOGY
Due to different and unknown reasons —- injury to the layer of cells that line the small blood vessels of the lungs —- may cause changes in the way these cells interact with the smooth muscle cells in the vessel wall. As a result, the smooth muscle contracts more than normal —- pulmonary arteries that carry blood from the heart to the lungs become narrowed —- making it difficult for blood to flow through the vessels —- as a result, high blood pressure in pulmonary arteries —- this abnormally high pressure strains the right ventricle of the heart —- causing it to expand in size —- overworked and enlarged —- right ventricle gradually becomes weaker and loses its ability to pump enough blood to the lungs —- leads to the development of right heart failure
CLINICAL MANIFESTATIONS
- Fatigue
- Dizziness
- Fainting spells
- Swelling in the ankles, abdomen or legs
- Bluish lips and skin
- Chest pain
- Irregular heartbeat (palpitations or strong, throbbing sensation)
- Tachycardia
- Progressive shortness of breath
DIAGNOSTIC TESTS
- Physical examination
Listen for abnormal heart sounds, such as a loud pulmonic valve sound, a systolic murmur of tricuspid regurgitation, or a gallop due to ventricular failure
Examine the jugular vein in the neck for engorgement
Examine the abdomen, legs, and ankles for fluid retention
Examine nail beds for bluish tint
Look for signs of other underlying diseases that might be causing pulmonary hypertension
- Blood tests
Complete metabolic panel (CMP): examines liver and kidney function
Autoantibody blood tests, such as ANA, ESR, and others: screens for collagen vascular diseases
Thyroid stimulating hormone (TSH): a screening for thyroid problems
HIV: a screening for human immunodeficiency virus
Arterial blood gases (ABG): determines the level of oxygen in arterial blood
Complete blood count (CBC): tests for infection, elevated hemoglobin, and anemia
B-type natriuretic peptide (BNP): a marker for heart failure
- Doppler echocardiogram: uses sound waves to show the function of the right ventricle to measure blood flow through the heart valves, and then calculate the systolic pulmonary artery pressure
- Chest X-ray: shows an enlarged right ventricle and enlarged pulmonary arteries
- 6-minute walk test: determines exercise tolerance level and blood oxygen saturation level during exercise
- Pulmonary function tests: evaluates for other lung conditions, such as chronic obstructive pulmonary disease and idiopathic pulmonary fibrosis among others
- Polysomnogram or overnight oximetry: screens for sleep apnea (results in low oxygen levels at night)
- Right heart catheterization: measures various heart pressures (i.e. inside the pulmonary arteries, coming from the left side of the heart), the rate at which the heart is able to pump blood, and finds any leaks between the right and left sides of the heart
- Ventilation perfusion scan (V/Q scan): looks for evidence of blood clots along the pathway to the lungs
- Pulmonary angiogram: looks for blood clot blockages in the pulmonary arteries
- Chest CT scan: looks for blood clots and other lung conditions
MANAGEMENT
Nonpharmacological Management
- Appropriate diagnosis and analysis of the problem is necessary before starting any treatment. Treatment varies per individual based on the different underlying causes but generally includes taking medications; making lifestyle and dietary changes
- Oxygen therapy: replaces the low oxygen in blood
- Nutrition: fuel the body with a nutritious diet that is low in fat, cholesterol and sodium and rich in high-fiber, whole grain, foods, including fruits and vegetables and lean protein
- Physical activities: regular activity may help improve the ability to be active
- Smoke-free living: quit smoking. Avoid second hand smoking. Smoking and breathing second-hand smoke make PPH symptoms worse
Pharmacological Management
- Anticoagulants or ‘blood thinners’ such as warfarin sodium. It decreases blood clot formation, so blood flows more freely through blood vessels
- Diuretics: furosemide, spironalactone, removes extra fluid from the tissues and bloodstream, which reduces swelling and makes breathing easier
- Potassium: replaces potassium that may be lost with increased urination when taking diuretics
- Inotropic agents (such as Digoxin): improves the heart’s pumping ability
- Vasodilators and calcium channel blockers (Nifedipine or diltiazem): lowers pulmonary blood pressure and may improve the pumping ability of the right side of the heart
- Endothelin receptor antagonists (bosetan): these help block the action of endothelin, a substance that causes narrowing of lung blood vessels
- Prostaglandins (epoprostenol): dilates pulmonary arteries and helps prevent blood clots from forming
- Phosphodiesterase type 5 inhibitors (sildenafil): relax pulmonary smooth muscle cells, which further leads to dilation of the pulmonary arteries
Surgical Management
- Atrial septostomy: it is a surgical procedure that creates a communication between the right and left atria. It relieves pressure on the right side of the heart, but at the cost of lower oxygen levels in blood (hypoxia)
- Pulmonary thromboendarterectomy: if present, a large clot in the pulmonary artery may be surgically removed to improve blood flow and lung function
- Lung transplantation: currently, this is the only cure for primary pulmonary hypertension. Transplantation is reserved for advanced pulmonary hypertension that is not responsive to medical therapy. The right side of the heart will generally return to normal after the lungs have been transplanted
- Heart/lung transplantation: this type of double organ transplant is very rare but is necessary for all patients who have combined lung and left heart failure
COMPLICATIONS
- Right-sided heart failure (Cor pulmonale): in cor pulmonale, heart’s right ventricle becomes enlarged and has to pump harder than usual to move blood through narrowed or blocked pulmonary arteries. At first, the heart tries to compensate by thickening its walls and expanding the chamber of the right ventricle to increase the amount of blood it can hold. But this thickening and enlarging works only temporarily, and eventually the right ventricle fails from the extra strain
- Blood clots: a number of small clots or just a few large ones dislodge from these veins and travel to the lungs, leading to a form of pulmonary hypertension that is reversible with time and treatment
- Arrhythmia: irregular heartbeats (arrhythmias) from the upper or lower chambers of the heart are complications of pulmonary hypertension. These can lead to palpitations, dizziness or fainting and can be fatal
- Bleeding: pulmonary hypertension can lead to bleeding into the lungs and coughing up blood (hemoptysis). This is another potentially fatal complication
NURSING MANAGEMENT
Nursing Assessment
- Note the changes suggesting increased work of breathing or pulmonary edema
- Assess breathing sound
- Assess sign of hypoxemia and hypercapnea
- Analyze the ABG and compare the previous values
- Determine hemodynamic status and compare it with previous value
Nursing Diagnosis
- Impaired gas exchange related to inadequate respiratory centre activity or chest wall movement, airway obstruction, or fluid in lung
- Ineffective airway clearance related to increased or tenacious secretion
- Acute pain related to inflammatory process and dyspnea
- Anxiety related to pain dyspnea and serious condition
Nursing Intervention
- Improve gas exchange:
Administer oxygen to maintain PaO2 of 60 mm Hg, using devices that provide increased oxygen concentration
Monitor fluid balance by intake and output measurement, urine-specific gravity. Daily weight measurement
Provide measures to prevent atelectasis and promote chest extension and secretion clearance as per doctor’s prescription spirometer
Elevate head level to 30 degrees
Monitor adequacy of alveolar ventilation by frequent measurement of respiratory system
Administer antibiotic, cardiac medication, and diuretics as prescribed by doctor
- Maintain airway clearance:
Administer medication to increase alveolar function
Perform chest physiotherapy to remove mucus
Administer IV fluids
Suction patient as needed to assist with removal of secretions
- Relieving pain:
Watch patient for sign of discomfort and pain
Position the head elevated
Give prescribed morphine and monitor for pain relieving sign
- Reducing anxiety
Correct dyspnea and relieve physical discomfort
Speak calmly and slowly
Explain diagnostic procedure