NURSING PROCESS – Definition, Steps, Assessment, Diagnosis, Planning, Implementation and Evaluation
DEFINITION
Nursing process is an orderly, systematic manner of determining the patient’s problems, making plans to solve them, initiating the plan or assigning others to implement it and evaluating the extent to which the plan was effective in resolving the problems identified.
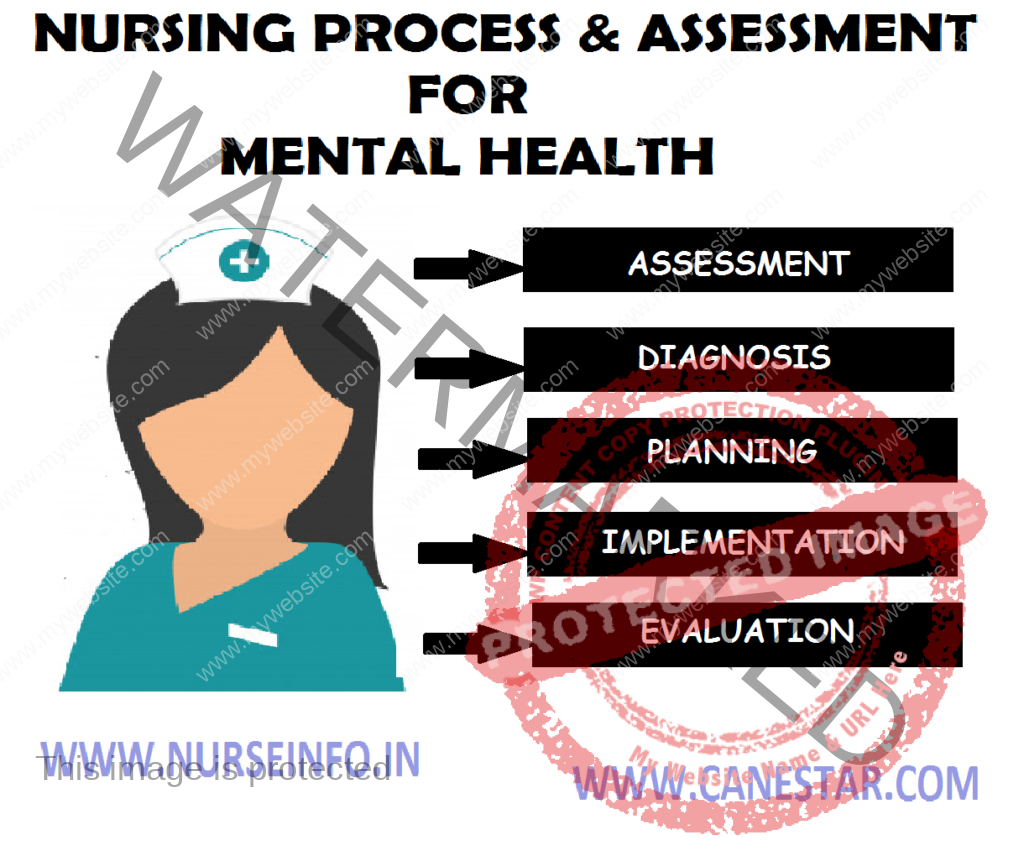
The five steps in nursing process are as follows:
- Assessment or gathering data
- Diagnosis or identifying a problem
- Planning or creating a plan to achieve desired outcomes
- Implementation or enacting the plan
- Evaluation or determining the effectiveness of the plan
NURSING ASSESSMENT
Assessment involves the collection, organization and analysis of information about the patient’s health. In psychiatric mental health nursing, this process is often referred to as a psychosocial assessment. The nurse obtains assessment data from several sources.
Components of Psychosocial Assessment
- Interview with the patient and his family
- History and physical examination
- Mental status examination
- Records from other healthcare facilities or prior treatment
- Laboratory and psychological tests
- Assessments by other professional and para-professionals
Clinical Interview
The interview allows the nurse to hear the patient’s perspective on the problem
- Conduct the interview in a quiet place, ensure privacy
- Be relaxed and maintain an unhurried posture
- Maintain eye contact with the patient
- Be interested and attentive to what he says
- Pick up verbal and non verbal cues of distress
- Allow the patient to talk freely without any interruption
- When the patient deviates from the theme or loses his tract, guide him to the main theme politely
- Use open-ended questions
- Use active listening
- Do not offer premature conclusions and assurance on the outcome of the treatment
History Taking
History taking proceeds through different headings as follows:
- Identification and demographical details
- Presenting complaints and duration
- History of present illness
- Past psychiatric history
- Family history
- Personal history
- Premorbid personality
Identification and Demographical Details
This includes the patient’s name, age, sex, religion, address, socioeconomic status, hospital number, marital status, occupation details of informant, and information relevant or not, adequate or not.
Presenting Complaints/Chief Complaints
Here symptoms are listed in a chronological order with their duration. Sometimes the patient may deny the existence of any symptoms and say that he was forcibly brought to the hospital by his relatives. In such cases, information is collected from his relatives. It is preferable to use the patient’s own words verbatim, without translating or interpreting their meaning. For example, sleeplessness – 3 weeks, loss of appetite and hearing voices – 2 weeks.
The mode of onset of the illness may be acute or insidious. The progress may be steady and progressive or diminishing and reappearing periodically or staying the same way throughout. These should also be enquired into. Sometimes the patient will be able to point out some antecedent stressful event alluded as precipitants. The temporal relation of the event with the illness, severity of the stress, the patient’s preoccupation with the events and the value attached to the event by him, may all give a clue to the presence and nature of the precipitant.
History of Present Illness
Under this are recorded the evolution of the patient’s symptoms from the time they were first noted till the time of consultation. Details of each symptom should be collected. The patient’s history may have to be supplemented with data available from other sources.
It is ideal to use the patient’s own words. Look for and also ask for any precipitating factors. An attempt should also be made to identify any possible secondary gain to the patient because of his symptoms.
Past Psychiatric History
Enquire whether the patient has any psychiatric illness in the past. If so its nature, duration, treatment and outcome should be noted down. If treatment was discontinued in the middle enquire the reason for this as well as the reason for switching over to other models of therapy.
Family History
Enquire about the type and size of family and the general family environment. The presence of psychiatric illness on the paternal or maternal side should be routinely asked. It would be useful to construct a family tree depicting the living members, their age, deceased members and their age at death. Mark whether any of them has or had a similar illness and if known the type of treatment they received and the outcome. Note specifically any history of suicide, mental retardation, epilepsy or any genetically transmittable disorders.
Personal History
The personal history includes the developmental, educational, occupational as well as the sexual history of the patient. Developmental history includes details of pregnancy and delivery, developmental milestones, health during childhood and adolescence, neurotic symptoms and occurrence of any significant event (for example, separation from parents, bereavements, etc are recorded).
The educational history relates to details regarding the level of performance in school, relationship with peers and teachers, academic achievements and extracurricular activities.
In occupational history, enquiry should be made about the types of work, job satisfaction, whether jobs were changed frequently and if so, the reasons for this, work skills and relationship with colleagues.
Sexual history includes details about sexual development, practices and attitudes towards sex. In marital history, enquire about married life and details about spouse and children.
Premorbid Personality
Personality of a patient consists of those habitual attitudes and patterns of behavior which characterize an individual. Personality sometimes changes after the onset of an illness. The nurse has to get a description of the personality before the onset of the illness and aim to build up a picture of the individual not a type. Enquiry with respect to the following areas has to be made.
- Attitude to others in social, family and sexual relationship: Ability to trust others, make and sustain relationship, anxious or secure, leader or follower, participation, responsibility, capacity to make decision, dominant or submissive, friendly or emotionally cold, etc. Difficulty in role taking- gender, sexual and familial.
- Attitude to self: Egocentric, selfish, indulgent, dramatizing, critical, depreciatory, over concerned, self-conscious, satisfaction or dissatisfaction with work. Attitude towards health and bodily functions. Attitude to past achievements and failure, and to the future.
- Moral and religious attitudes and standards: Evidence of rigidity or compliance, permissiveness or over conscientiousness, conformity, or rebellion. Enquire specifically about religious beliefs. Excessive religiosity
- Mood: Enquire about stability of mood, mood swings, whether anxious, irritable, worrying or tense. Whether lively or gloomy. Ability to express and control feelings of anger, anxiety or depression.
- Leisure activities and hobbies: Interest in reading, playing, music, movies, etc., Enquire about creative ability. Whether leisure time is spent alone or with friends. Is the circle of friends large or small?
- Fantasy life: Enquire about content of day dreams and dreams, amount of time spent in day dreaming
- Reaction pattern to stress: ability to tolerate frustrations, losses, disappointments, and circumstances arousing anger, anxiety or depression. Evidence for the excessive use of particular defense mechanisms, such as denial, rationalization, projection, etc.,
Mental Status Examination
The mental status examination (MSE) is used to determine whether a patient is experiencing abnormalities in thinking and reasoning ability, feelings or behavior. The MSE includes observations and questions in the following categories:
- General appearance and behavior
- Speech
- Thought
- Mood and affect
- Perception
- Cognitive functions
General Appearance and Behavior
Describe patient’s appearance and behavior. Is he dressed properly? Assess the patient’s sensorium. Is he alert? Drowsy? Stuporous? Comatose? Is he cooperative for the examination? Does he make eye contact with the examiner? What is his level of activity? Is he excited? Retarded? Hyperactive? Restless? Does he have any mannerisms? Gestures? Tics? Involuntary movements?
Speech
The manner of speaking and its defects are recorded under speech, whereas the content and form of speech are recorded under thought disorders. Does he speak spontaneously or only responding to questions posed to him? Assess the rate, quantity and flow of speech. It is worthwhile to record a sample of speech for later analysis.
Thought
Inference about the thought process and its disorders are made from the speech sample or the writing sample of the patient. Disorders of form, progression, content and possession may be present. Does the patient have delusions, obsessive ruminations and thought alienation? How does the delusion affect his behavior?
Mood and Affect
The patient should be asked about his affective state. Compare the subjective report with what is objectively observed. Is his mood appropriate or not? Congruent or incongruent? Labile? Is the emotional expression blunt? Is the emotional expression blunt? Is the affective expression adequate and appropriate?
Perception
Has the patient any perceptual abnormalities like illusions and hallucinations? If hallucinating, what is the type of hallucination and what is his reaction?
Cognitive Function
Is the patient attentive? Can his attention be easily aroused and sustained? How is his concentration? To assess cognitive function some simple tests can be administered. The patient is asked to name the days of the week or names of the months forwards and backwards. He may be asked to serially subtract 7 or 3 from 100 and tell the numbers.
Is the patient oriented to time, place and other persons? Orientation to time involves ability to tell correctly the time of the day, date, week, month, year and other related data. Orientation to a place includes correct information of his whereabouts, how he came to be there and other details. Correct identification of people around him ensures orientation to other persons.
Patient’s intelligence can be inferred from his conversation and behavior, educational level vocabulary, ability for abstract thinking and reasoning, general information, etc., Specific tests are used when a more accurate measurement of intelligence is needed. The patient’s awareness of his disabilities and readiness for treatment are reflected in insight. Judgment may be inferred from his plans for the future.
Physical Examination
A thorough physical examination should be carried out in all cases. The physical examination should include body system review, neurological status and laboratory tests.
Particular attention is paid to recent head trauma, episodes of hypertension, and changes in personality, speech, or ability to handle activities of daily living. Also note for any movement disorders. Available laboratory data are reviewed for any abnormalities and documented. Particular attention is paid to any abnormalities of hepatic or renal function because these systems metabolize or excrete many psychiatric medications. In addition, abnormal white blood cell and electrolyte levels should be noted.
Psychological Tests
Psychological tests are another source of data for the nurse to use in planning care for the patient. Commonly used psychological tests are instruments for assessing symptoms.


Thanks