FAT SOLUBLE VITAMINS – VITAMIN A – Deficiency, Clinical Features, Treatment, Prevention and Toxicity
Vitamins are organic substances which have to be supplied in food in minute quantities to maintain the biochemical and structural integrity of many cells and tissues. The human body cannot synthesize them. Most of them are integral parts of certain coenzymes required for biochemical reactions at tissue levels.
The vitamins have been classified into fat-soluble and water-soluble groups based on their presence in natural foods. By synthetic processes water soluble, preparations of some of the fat soluble vitamins have been produced, e.g. vitamin K. The fat-soluble vitamins are A, D, E and K. The water-soluble vitamins are C and B complex group consisting of thiamine, niacin, riboflavin, pyridoxine, biotin, cyanocobalamin, folic acid and pantothenic acid.
VITAMIN A
Vitamin A has a crucial role in normal visual processes and the maintenance of health of epithelial cells. Deficiency of vitamin A is one of the major causes of preventable blindness occurring in many developing countries. This deficiency is widely prevalent in India and about 10% of school children are affected. Its prevalence is higher in the southern states.
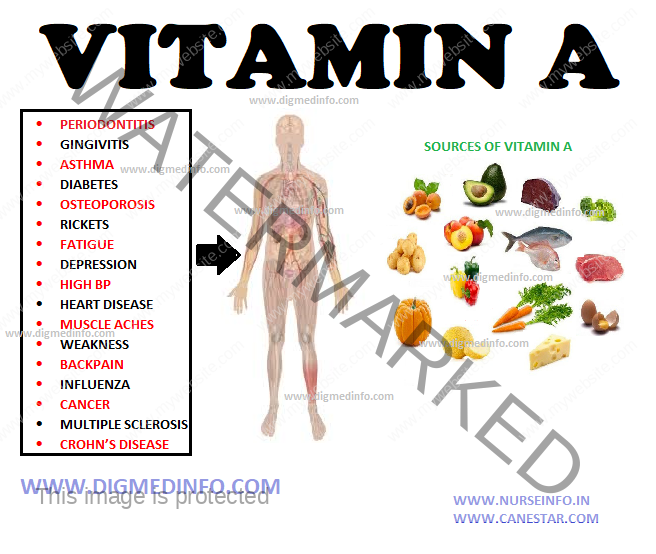
Source of intake Vitamin A is found exclusively in animal foods. Rich sources of animal origin are liver, especially fish, liver, butter, ghee, cheese, egg yolk, and milk. Vegetable sources contain the precursor for vitamin A, i.e. carotene especially beta carotene. Rich sources of carotene include dark green leafy vegetables such as spinach and amaranth, yellow vegetables like carrot and pumpkin, and fruits like mangoes and papaya. Red palm oil is a very rich source of carotene. In the body carotene is converted into vitamin A. Six parts of carotene are equivalent to one part of vitamin A. Vitamin A is stable at temperatures below 100°C. Vitamin A is stored in the liver as retinyl esters and these stores can last for 6-9 months.
DEFICIENCY
Dryness of the eyes leads to xerophthalmia. Bitot’s spots develop as whitish scaly plaques on the sclera and they consist of heaped up metaplastic epithelium. The cornea softens, opacifies, ulcerates and necroses and this condition is called keratomalacia. This leads to blindness. Even in subclinical vitamin A deficiency the conjunctival epithelium shows changes in 90-95% of cases. The conjunctiva is made up of epithelial and goblet cells. Conjunctival impression cytology using a multipore filter (pore size 0.45/μm) applied to the conjunctiva for 2-3 minutes is diagnostic. On staining this with PAS, the epithelial abnormality can be made out.
A dose of 1 μg, of retinol is equivalent to 3 international units of vitamin A and 6 μg of carotenoids. An additional 400 μg should be provided during lactation. Primary vitamin A deficiency generally results from inadequate intake of the vitamin or the carotenoids in the diet. Deficiency of other nutrients usually coexists. Secondary vitamin A deficiency occurs due to intestinal malabsorption, liver diseases like cirrhosis and enhanced renal excretion.
Clinical features
Earliest symptom is night blindness, followed by degenerative changes in the retina. The bulbar conjunctiva becomes dry, and rough greyish triangular foamy raised patches appear (Bitot’s spots). A solution
of 1% Rose Bengal instilled into the eye stains Bitot’s spots dark pink and makes them stand out prominently. Both night blindness and xerosis of the conjunctiva readily disappear on administering vitamin A. When the cornea also becomes dry and lusterless it is called xerophthalmia. More serious complications are keratomalacia involving the cornea with ulceration and necrosis. These changes follow if xerophthalmia is left untreated. Keratomalacia is more common in children aged 1-5 years. It leads to perforation, prolapse of the iris, and endophthalmitis leading to blindness. Skin changes include dryness and hyperkeratosis. A variety of infantile hydrocephalus has been attributed to vitamin A deficiency.
Vitamin A deficiency should be suspected in all malnourished children. Normal serum level of vitamin A is 20 μg/dL. Serum levels less than 10 μg/dL are indicative of deficiency. Several secondary benefits are attributable to proper Vitamin A nutritional status. Epidemiological studies report increased mortality due to diarrhea and measles in children who are deficient in Vitamin A.
Treatment
A mixed diet with adequate amount of protein is recommended. Vitamin A may be administered orally as retinol, 30 mg (9,000-10,000 IU) for 3 days. In more advanced cases retinol acetate or palmitate may be intramuscularly in a dose of 5000-10,000 units. The corneal lesions clear up within 48-72 hours. The vitamin preparation in a dose of 8-10 mg/day should be given for a month and thereafter maintenance dose of 1.5 mg/day should be continued regularly. Patients with ocular complications should be referred to the ophthalmologist.
Prevention
The diet should contain at least 100 g of green vegetables and adequate amounts of animal products. Occurrence of vitamin A deficiency in 5% or more of the population calls for mass treatment. In poor communities 60 mg retinol palmitate or acetate administered orally once in 6 months or 300,000 IU once a year under supervision
has been found to be extremely useful. Vitamin A deficiency occurring during pregnancy and lactation leads to poor vitamin A stores in the fetus and low vitamin A content of breast milk. These can be prevented by adequate supplementation during pregnancy. Treatment schedule for xerophthalmia for all agegroup-children
Overdosage of carotene
Excessive intake of carotene containing foods, principally carrots, leads to hypercarotenemia. It is a cosmetic problem due to yellowish pigmentation of skin. The serum is yellow but sclera is white. The pigmentation disappears with the elimination of excessive carotene from the diet. Hypothyroid patients are very susceptible to hypercarotenemia. Hypercarotenemia does not lead on to hypervitaminosis A.
Vitamin A toxicity
This may be due to self-medication or large scale ingestion of livers of fish or polar bear having enormous quantities of vitamin A. Acute toxicity Symptoms include abdominal pain, nausea, vomiting, headache, and desquamation of the skin. Recovery occurs spontaneously on removing the source of the vitamin from the diet.
Chronic toxicity
This is seen in people who take 40,000 units or more of vitamin A daily for a prolonged period. It is characterized by bodyaches, arthralgia, hair loss, anorexia, benign intracranial hypertension, weight loss and hepatomegaly. Chronic overdose of Vitamin A may be associated with osteoporosis and increased incidence of hip fractures, have been reported in Scandinavian countries.
Clinical diagnosis can be confirmed by demonstrating raised vitamin A concentration in the serum and normal retinol binding protein. Withdrawal of the vitamin from the diet brings about prompt relief.