ENDOSCOPIC RETROGRADE CHOLANGIOPANCREATOGRAPHY – Purpose, Indications, Client Preparation, Procedure, Post-Procedural Care, Factor Affecting Diagnostic Results and Client Teaching
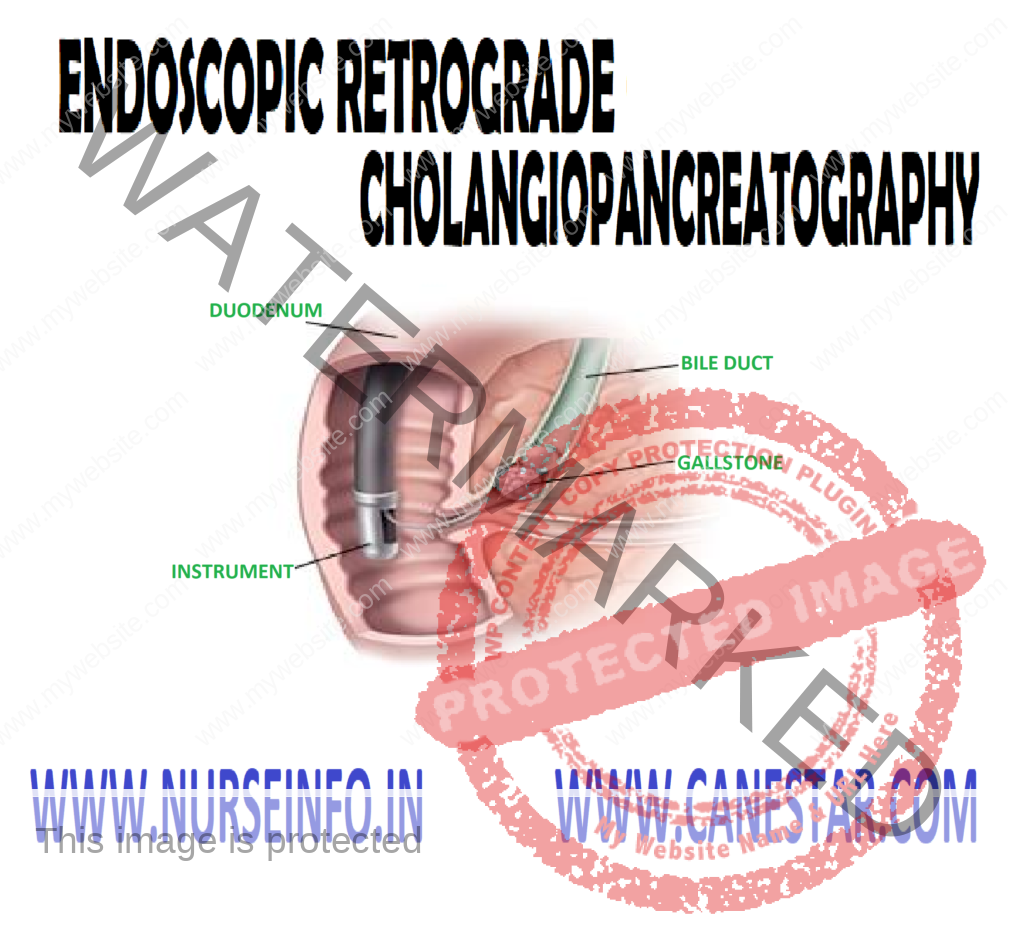
Endoscopic retrograde cholangiopancreatography (ERCP) is an imaging in which the biliary pancreatic ducts are examined endoscopically after contrast medium is injected into the duodenal papilla.
The purpose of this procedure is to identify the cause of a biliary obstruction, which could be stricture, cyst, stones, or tumor; jaundice is usually present. ERCP is performed following abdominal ultrasound, computed tomography, liver scanning and/or biliary tract X-ray studies to confirm or diagnose hepato-biliary or pancreatic disorders.
PURPOSE
- To detect biliary stones, strictures, cyst or tumor
- To identify biliary obstruction, such as stones or strictures
- To confirm a biliary or pancreatic disorders
INDICATIONS
- Biliary stones
- Biliary strictures, cyst or tumor
- Primary cholangitis
- Cirrhosis
- Pancreatic stones
- Stricture, cysts, or pseudocyst or tumor
- Chronic pancreatitis
- Pancreatic fibrosis or duodenal papilla tumors
CLIENT PREPARATION
- Obtain a client history of allergies to seafood, iodine and contrast dye. Report allergic findings
- Determine whether the anxiety level may interfere with the client’s ability to absorb information concerning the procedure
- Check that the consent form has been signed prior to premeditations
- Explain to the client that when the contrast medium is injected, there usually is a transient flushing sensation
- Be supportive of the client prior to and during the test procedure
- Explain to the client that when the contrast medium is injected, there usually is a transient flushing sensation.
- Be supportive of the client prior to and during the test procedure
- Monitor the vital signs during the test and compare them to baseline vital signs. An increase in the pulse rate could be due to atropine. Rupture within the gastrointestinal tract caused by endoscope perforation could cause shock
- Inform the client that the endoscope will not obstruct breathing
- Inform the client that atropine will make the mouth dry and the tongue feels large or swollen
- Inform the client that the test takes approximately 1 hour and that lying still on the X-ray table is important
PROCEDURE
- Food and fluids are restricted for at least 8 hours before the test
- The consent form should be signed prior to premeditation
- Obtain baseline vital signs. Have the client void
- Premedicate with mild narcotic or sedative. Atropine may be given prior to or after insertion of the endoscope. Atropine relaxes gastrointestinal motility and will cause dryness of mouth
- Local anesthetic is sprayed in back of throat (pharynx) to decrease the gag reflex prior to the insertion of the fiberoptic endoscope
- Secretion may be given intravenously to paralyze the duodenum. Contrast medium is injected after the endoscope is at the duodenal papilla and the catheter is in the pancreatic duct
POST-PROCEDURAL CARE
- Monitor vital signs. A rise in temperature might indicate (bacteremia or septicemia). Check respirations for respiratory distress resulting from anesthetic spray and/or the endoscope
- Check the skin color. Increased or decreased jaundice is an indicator of a disease process or the result of therapy
- Check the gag reflex before offering food or drink
- Check signs and symptoms of urinary retention caused by atropine
FACTOR AFFECTING DIAGNOSTIC RESULTS
Inability to cannulate biliary and/or pancreatic duct
CLIENT TEACHING
- Suggest warm saline gargle and/or lozenges to decrease throat discomfort
- Explain to the client that he or she has a sore throat for a few days after the rest. This is due to the endoscope