ABDOMINAL HERNIA – Etiology and Risk Factors, Signs and Symptoms, Types, Diagnostic Evaluation and Management
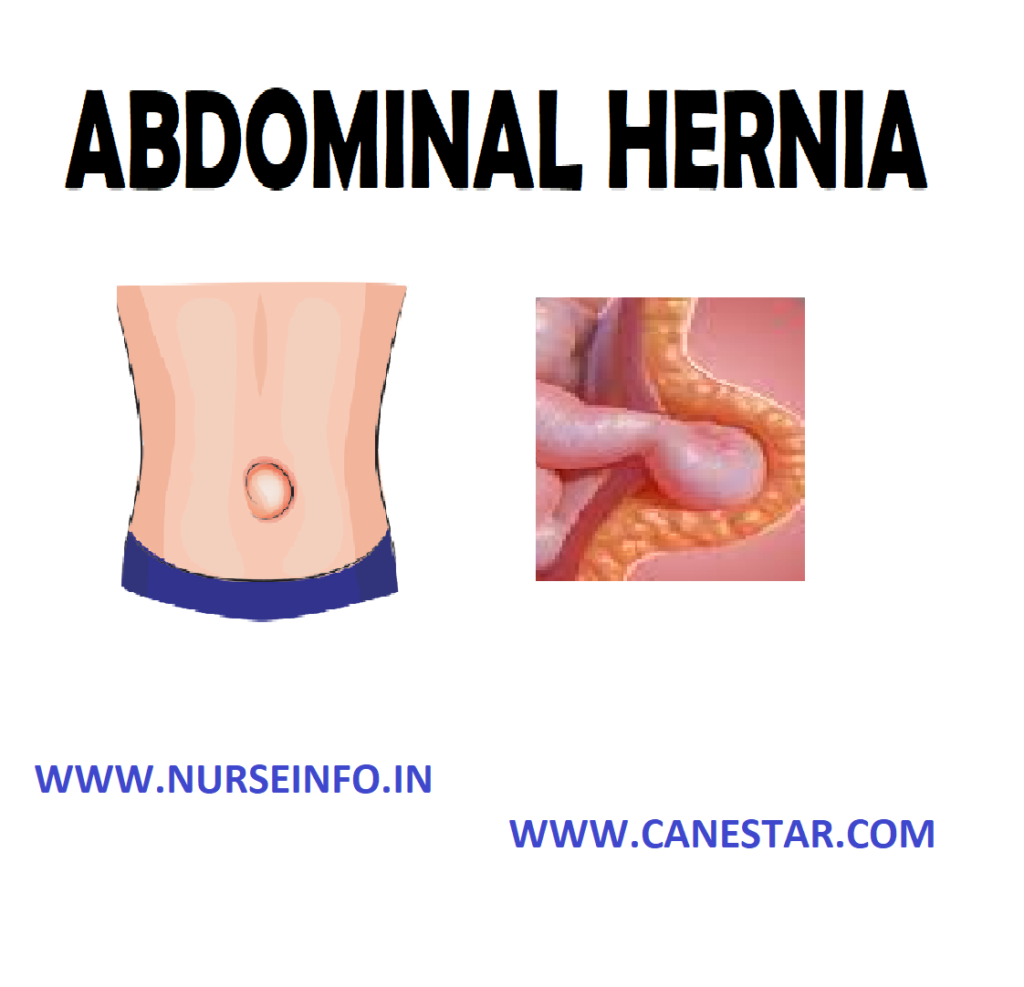
In general, hernia refers to a condition that arises when an organ pushes through a weak area in the muscles or tissue that surrounds and contains it.
An abdominal hernia occurs when there is a tear in the inner lining of the abdominal wall (the outer layer of muscle, fat and tissue that extends from the bottom of the ribs to the top of the thighs), causing a bulge in the abdominal wall where the organs protrude
The bulge can be either reducible, which means that by applying slight pressure to the area, the organs are being pushed back into the abdominal cavity and the hernia will flatten and disappear, or non-reducible, which means the fat or tissue cannot be pushed back into the abdomen and the hernia will not flatten
ETIOLOGY AND RISK FACTORS
A hernia can develop in anyone, from a newborn baby to a senior citizen. The following may increase risk of developing a hernia by increasing pressure on the abdominal wall:
- A chronic cough, such as smoker’s cough
- Obesity
- Straining during bowel movements or while urinating
- Pregnancy
- Straining to lift heavy objects
- Persistent sneezing, such as that caused by allergies
- Prolonged seating or standing
The risk of having an abdominal hernia increases with age because the older you get, the weaker your abdominal wall muscles become
SIGNS AND SYMPTOMS
- The main sign of an abdominal hernia is having a bulge or swelling appear on a part of abdomen. Often, the bulge will disappear in lying down position or push on it and then reappear during standing, cough or sneeze. This is called a reducible hernia
- Other symptoms are burning, slight discomfort and a feeling heaviness or aching in abdomen
TYPES OF ABDOMINAL HERNIAS
The following are different types of abdominal hernia:
Inguinal Hernia
When a male’s testicles descend into the scrotum, this causes a naturally weakened area in the wall of the abdomen, called the internal ring. This weakened area makes men more susceptible to a hernia at this location.
It is of two types:
- Indirect inguinal hernia: an indirect inguinal hernia is the most common type of inguinal hernia. It occurs at the internal ring in the groin area. The intestine drops down into the internal ring and can extend down into the scrotum in men or to the outer folds of the vagina in women. An indirect inguinal hernia can be the result of an inherited weakness at the internal ring or one that occurs later in life. The latter is known as an acquired hernia
- Direct inguinal hernia: less common than an indirect inguinal hernia, a direct inguinal hernia occurs near the internal ring instead of within it. They are acquired hernias that usually occur after age 40 as a result of aging or injury
Epigastric Hernia
This type of hernia occurs as a result of a weakness in the muscles of the upper-middle abdomen, above the navel. Men are about three times more likely to have an epigastric hernia than women
Umbilical Hernia
They involve protrusion of intra-abdominal contents through a weakness at the site of passage of the umbilical cord through the abdominal wall. These hernias often resolve spontaneously. Umbilical hernias in adults are largely acquired, and are more frequent in obese or pregnant women. Abnormal decussation of fibers at the linea alba may contribute. These hernias can occur in babies, children and adults
Femoral Hernia
Femoral hernias occur just below the inguinal ligament, when abdominal contents pass into the weak area at the posterior wall of the femoral canal. They can be hard to distinguish from the inguinal type. It occurs in the area between the abdomen and the thigh, and appears as a bulge on the upper thigh. This type of hernia is more common in women than men.
Incisional Hernia
An incisional hernia occurs when the defect is the result of an incompletely healed surgical wound. It can occur at the site of an incision from a previous surgery. The fat or tissue pushes through a weakness created by the surgical scar. An incisional hernia can occur months or years after the initial surgery
Diaphragmatic Hernia
Higher in the abdomen, diaphragmatic hernia results when part of the stomach or intestine protrudes into the chest cavity through a defect in the diaphragm. A hiatus hernia is a particular variant of this type, in which the normal passageway through which the esophagus meets the stomach (esophageal hiatus) serves as a functional “defect”, allowing part of the stomach to herniated into the chest.
DIAGNOSIS OF ABDOMINAL HERNIA
- By taking history
- Physical examination
- Examine the bulge or swelling
- Ultrasound scan
- X-rays
- CT scan
MANAGEMENT
Non-Surgical Treatment
Treatment for hernias can be surgical or nonsurgical, depending on their severity. Non-surgical treatments usually help ease pain and discomfort caused by a hernia but do not correct the problem.
Trusses
There are two kinds of trusses for hernias, the spring truss and the umbilical truss. The spring truss is worn around the waist and acts as a support, while the umbilical truss is worn around the midsection. Trusses also come in different sizes and are usually worn under briefs.
Hernia Belts
Hernia belts are lightweight and made in such a way that movement is not restricted while you are recovering. These belts were designed to be worn over briefs, are made with adjustable straps and are lined with foam for extra comfort. The foam compression pads provide gradual pressure and support to the weakened muscles
Bindings
Abdominal bindings are made of elastic and provide uniform compression and support of the abdominal muscles. They can be fastened around the waist.
Hernia Briefs
Hernia briefs look like regular briefs except they are made with spandex and foam pads for extra support and are designed to provide rupture relief. The material is convenient because it is lightweight, cool and washable and is easy to wear. It is important to remember that these nonsurgical treatments for hernias are not meant to correct the problem. They are only meant to provide comfort and pain-relief for those engaged in physically demanding tasks.
Surgical treatment: surgery of hernia can be performed through various approaches;
- Herniotomy
- Herniorrhaphy
- Hernioplasty
- Laparoscopy
- Herniotomy (removal of the hernia sac only) alone is adequate for an indirect inguinal hernia in children in whom the abdominal wall muscles are normal.
- Herniorrhaphy (herniotomy plus repair of the posterior wall of the inguinal canal) may be suitable for a small hernia in a young adult with good abdominal wall musculature.
- Hernioplasty (reinforcement of the posterior inguinal canal wall with a synthetic mesh) is required for large hernias in the middle-aged and elderly with poor abdominal wall musculature.
- Laparoscopic hernia repair surgery: during a laparoscopic hernia repair, a surgeon makes small incisions in the abdominal wall, and the abdomen is inflated with carbon dioxide. A laparoscope (a thin, tube-like instrument with a small video camera) and surgical instruments are then inserted through the incisions. While viewing a monitor, the surgeon pushes the herniated intestine back into place and repairs the hernia opening with surgical staples. Mesh is then placed over the defect to reinforce the abdominal wall.
NURSING INTERVENTIONS
- Find out the recurrent coughing or sneezing causing symptoms and treat them
- Encourage not to strain too much on the toilet. Encourage to eat enough fruit and vegetables and increase fiber intake
- Also encourage to drink enough fluids
- Encourage to maintain a healthy weight
- Encourage exercising to tone the muscles of the abdomen
- Provide medical help for chronic constipation, allergies or a chronic cough
- Encourage not to be heavy work that will increase the intra-abdominal pressure
- Prepare the patient for diagnostic tests as needed
- Administer prescribed antacids and other medications
- To reduce intra-abdominal pressure and prevent aspiration, have the patient sleep in a reverse Trendelenburg position with the head of the bed elevated.
- Assess the patient’s response to treatment
- Observe for complications, especially significant bleeding, pulmonary aspiration, or incarceration or strangulation of the herniated stomach portion
- After endoscopy, watch for signs of perforation such as falling blood pressure, rapid pulse, shock, and sudden pain caused by endoscope
- To enhance compliance, teach the patient about the disorder. Explain significant symptoms, diagnostic tests, and prescribed treatments.
- Review prescribed medications, explaining their desired actions and possible adverse effects
- Teach the patient dietary changes to reduce reflux
- Encourage the patient to delay lying down for 2 hours after eating