ANEMIA – Etiology, Classification, Clinical Manifestations and Management
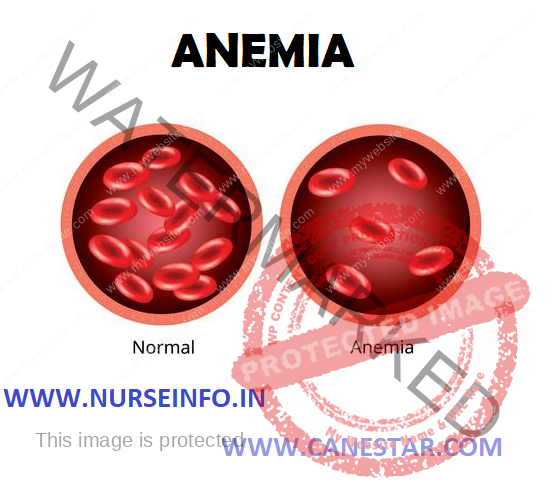
Anemia is a reduction in red blood cells (erythrocytes) which in turn decreases the oxygen carrying capacity of the blood. Anemia reflects on abnormality in RBC number, structure and function.
ETIOLOGY
- Loss of RBC’s: Occurs with bleeding, potentially from a major source, such as the gastrointestinal tract, the uterus, the nose, or a wound.
- Decreased production of RBC’s: Can be caused by a deficiency in cofactors (including folic acid, vitamin B12 and iron) required for erythropoiesis, RBC production may also be reduced if the bone marrow is suppressed (e.g. by tumor, medication, toxin) or is in adequately stimulated because of a lack of erythropoietin (as occur in chronic renal disease).
- Increased destruction of RCB’s: May occur because of an overactive RES(reticuloendothelial system) or because the bone marrow produces abnormal RCB’s that are then destroyed by the RES (sickle cell anemia)
CLASSIFICATION OF ANEMIA
- Morphologic
- Etiologic
Morphologic Classification:
- Normocytic, normochromic
- Macrocytic, normochromic
- Microcytic, hypochromic
Etiological Classification:
Decreased erythrocyte production (hypoproliferative anemia)
- Decreased hemoglobin production
- Iron Deficiency
- Thalassemias
- Defective DNA synthesis
- Cobalamin deficiency
- Folic acid deficiency
- Decreased number of erythrocyte
precursors
- Aplastic anemia
- Chronic diseases
- Chemotherapy
- Blood loss
- Acute : Trauma, blood vessel rupture
- Chronic: Gastritis, menstrual flow, hemorrhoids
Increased erythrocyte destruction (hemolytic anemia)
- Intrinsic: Abnormal hemoglobin (sickle cell anemia), enzyme deficiency (G-6-PD)
- Extrinsic: Physical trauma, medications, and toxins
IRON DEFICIENCY ANEMIA
Iron deficiency anemia typically results when the intake of dietary iron is inadequate for hemoglobin synthesis. The body can store about one fourth to one third of its iron, and it is not until those stores are depleted that iron deficiency anemia actually begins to develop. It is defined as anemia associated with either inadequate, absorption or excessive loss of iron; it is chronic, microcytic and hypochromic anemia.
ETIOLOGY
- In children, adolescents, and pregnant women, inadequate iron in diet; required to keep up with increased growth.
- For adults, blood loss (from ulcers, gastritis, inflammatory bowel disease, or gastrointestinal tumors)
- In premenopausal women, menorrhagia
- In chronic alcoholics, chronic blood loss from gastrointestinal tract
- Iron malabsorption after gastrectomy or with celiac disease
CLINICAL MANIFESTATION
Body System: Integumentary
Mild (10-14 g/dl): None
Moderate (6-10 g/dl): None
Severe (<6 g/dl): Pallor, jaundice, pruritis
Body System: Eyes
Mild (10-14 g/dl): None
Moderate (6-10 g/dl): None
Severe (<6 g/dl): Icteric conjunctiva and sclera, blurred vision
Body System: Mouth
Mild (10-14 g/dl): None
Moderate (6-10 g/dl): None
Severe (<6 g/dl): Glossitis, smooth tongue
Body System: cardiovascular
Mild (10-14 g/dl): Palpitation
Moderate (6-10 g/dl): increased palpitations, bounding pulse
Severe (<6 g/dl): tachycardia, systolic mummur, angina, MI
Body System: Pulmonary
Mild (10-14 g/dl): Exertional dyspnea
Moderate (6-10 g/dl): Dyspnea
Severe (<6 g/dl): Tachypnea, orthopnea, dyspnea
Body System: neurologic
Mild (10-14 g/dl): None
Moderate (6-10 g/dl): Roaring in ears
Severe (<6 g/dl): headache, vertigo, irritability, impaired though process
Body System: Gastrointestinal
Mild (10-14 g/dl): none
Moderate (6-10 g/dl): none
Severe (<6 g/dl): anorexia, hepatomegaly, splenomegaly, difficulty in swallowing, sore mouth
Body System: musculoskeletal
Mild (10-14 g/dl): none
Moderate (6-10 g/dl): none
Severe (<6 g/dl): bone pain
Body System: general
Mild (10-14 g/dl): none
Moderate (6-10 g/dl): fatigue
Severe (<6 g/dl): sensitivity to cold, weight loss, lethargy
DIAGNOSTIC EVALUATION
- History and physical examination:
- History:
Ask the patient for socioeconomic status, any injuries, any disease etc
- In physical examination check the vital signs temperature, pulse, respiration, blood pressure. Assess the skin color and signs of anemia. Check the body weight.
- History:
Ask the patient for socioeconomic status, any injuries, any disease etc
- Red blood cell size and color: with iron deficiency anemia, red blood cells are smaller and paler in color than normal
- Hematocrit: this is the percentage of blood volume made up by red blood cells. Normal levels are generally between 34.9 and 44.5 percent for adult women and 38.8 to 50 percent for adult men. These values may change depending on age.
- Hemoglobin: lower than normal hemoglobin levels indicate anemia. The normal hemoglobin range is generally defined as 13.5 to 17.5 grams (g) of hemoglobin per deciliter (dL) of blood for men and 12.0 to 15.5 g/dL for women. The normal ranges for children vary depending on the child’s age and sex.
- Ferritin: this protein helps store iron in body, and a low level of ferratin usually indicates a low level of stored iron
- Endoscopy: to check for bleeding from a hiatal hernia, an ulcer or the stomach with the aid of endoscopy
- Colonoscopy: to rule out lower intestinal sources of bleeding
- Ultrasound: women may also have a pelvic ultrasound to look for the cause of excess menstrual bleeding, such as uterine fibroids.
MANAGEMENT
To treat iron deficiency anemia, it is recommend taking iron supplements.
MEDICAL MANAGEMENT
- Oral iron preparations – ferrous sulfate, ferrous gluconate, and ferrous fumarate available
- In case, oral iron is poorly absorbed or poorly tolerated, or iron supplementation is needed in large amounts, intravenous or intra muscular administration of iron dextran needed.
- Before parenteral administration, a small test dose administered to avoid risk of anaphylaxis
- Emergency medications (e.g. ephinephrine) should be close at hand. If no signs of allergic reaction occurred after 30 minutes, remaining dose administered.
- IM injection causes local pain and stain skin. Side effects minimized by using Z-track technique for administering iron dextran deep into gluteus maximus muscle
- Because of problems with IM administration, IV route is preferred.
DIETARY MANAGEMENT
Foods rich in iron include:
- Red meat
- Pork
- Poultry
- Seafood
- Beans
- Dark green leafy vegetables, such as spinach
- Dried fruit, such as raisins and apricots
- Iron – fortified cereals, breads and pastas
- Peas
Choose foods containing vitamin C to enhance iron absorption
To enhance the body’s absorption of iron by drinking citrus juice or eating other foods rich in vitamin C at the same time. Vitamin C in citrus juices, like orange juice helps body to better absorb dietary iron.
Vitamin C is also found in:
- Broccoli
- Grape fruit
- Kiwi
- Leafy greens
- Melons
- Oranges
- Peppers
- Strawberries
- Tangerines
- Tomatoes