PAIN
Pain is often considered a fifth vital sign, assessed along with temperature, pulse, respiration, and blood pressure. Pain can affect patient’s physical, emotional, and mental well-being. It must be managed immediately and effectively so that they can perform daily activities
Pain can be acute or chronic. Acute pain is often severe with a rapid onset and a short duration. It generally resolves with healing. Chronic pain continues beyond the point of healing, often for more than 6 months. Cancer pain is in a category of its own. It can be acute, chronic, or intermittent and is caused by tumor growth and tissue necrosis
Principles of Pain Assessment and Management
- Patients have the right to appropriate assessment and management of pain (JCAHO Standard). Pain (should be) is assessed in all patients
- Pain is always subjective. Therefore, the patient’s self report of pain is the single most reliable indicator of pain. A clinician needs to accept and respect this self-report, absent clear reasons for doubt
- Physiological and behavioral (objective) signs of pain (e.g. tachycardia, grimacing) are neither sensitive nor specific for pain. Such observations should not replace patient self-report unless the patient is unable to communicate
- Assessment approaches, including tools, must be appropriate for the patient population. Special considerations are needed for patients with difficulty communicating. Family members should be included in the assessment process, when possible
- Pain can exist even when no physical cause can be found. Thus, pain without an identifiable cause should not be routinely attributed to psychological causes. Different patients experience different levels of pain in response to comparable stimuli. This is, uniform pain threshold does not exist
- Pain intolerance varies among and within individuals depending on factors including heredity, energy level, coping skills, and prior experiences with pain
- Patients with chronic pain may be more sensitive to pain and other stimuli. Unrelieved pain has adverse physical and psychological consequences. Therefore, clinicians should encourage the reporting of pain by patients who are reluctant to discuss pain, deny pain when it is likely present, or fail to follow through on prescribed treatments (JCAHO standard)
- Pain is an unpleasant sensory and emotional experience, so assessment should address physical and psychological aspects of pain
Characteristics of Pain
- Severity: ranges from no pain to excruciating pain
- Timing: duration and onset of pain
- Location: body area involved
- Quality: what the patient feels the pain is
- Personal meaning: how affects the persons daily life
Factors increasing and decreasing pain: age, gender, activity, rest, sleep, diet, culture, home remedies, drugs, alcohol, diversion activities like listening to music, watching TV, yoga, meditation, etc
Assessment of pain: assessment of pain can be done by under following headings:
- Location of pain
- Mode of onset (acute or chronic)
- Any precipitating factors
- Quality of pain (dull, moderate, shooting, spasms)
- Duration
- Any change in quality
- Any measures taken after pain started, if so
What measures?
Whether it is effective?
- Clinical observation
Client’s appearance
Motor behavior (facial expression, gait, posture)
Affective behavior
Local “observation” if pain is external
- Monitoring of vital signs like BP, pulse, temperature
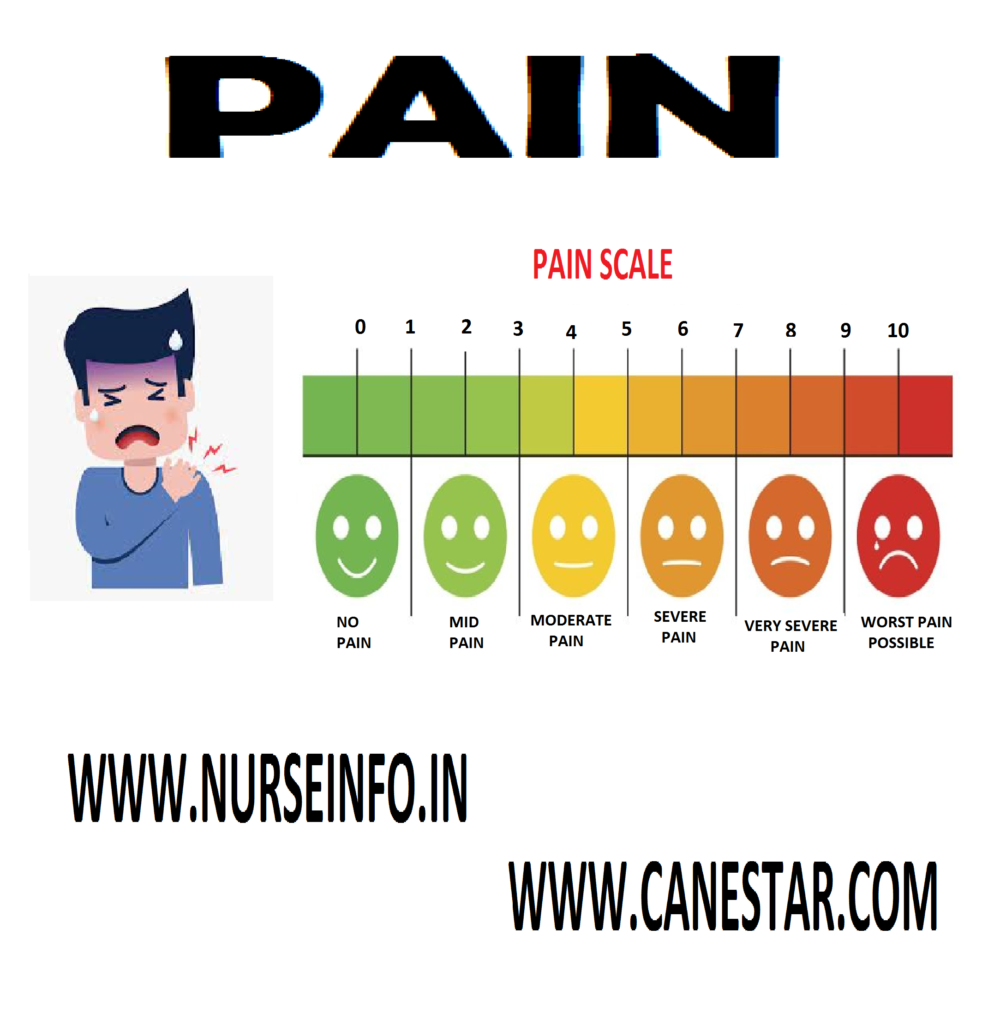
Pain assessment: pain intensity scale
Faces pain scale revised: this instrument has 6 faces depicting expressions that range from contented to obvious distress. The patient is asked to point to the face that most closely resembles the intensity of his or her pain
Management of pain: techniques used for management of pain
Few techniques are used to produce analgesia in the individuals. The common techniques used in the skin are:
- Pressure: pressure applied by fingertips or thumb
- Acupressure: it involves pressure and massage
- Massage: rubbing on and around the area of pain
- Cutaneous vibration: short and long wave diathermy
- Heat therapy: dry heat or moist heat application
- Cold therapy: dry cold or moist cold application
- External application: of gel or creams
- TENS (transcutenous electrical nerve stimulation) – using electrical current through electrodes applied to the skin surface of the painful region
- The mechanism involved in all above said techniques is according to pain theories available. Some of these techniques produce exogenous opiates to control the pain. Others block the endogenous pain inducing substances. There are few deep structures
Therapies used in pain management are:
- Acupuncture: it is a procedure, where needles are inserted at specific cutaneous sites. The effect is not immediate but opiates will be produced to control the pain
- Deep brain stimulation: here electrical stimulation is done to the certain areas of brain including frontal lobes, midbrain, caudate nucleus, etc
Drugs used in Pain Management
- Analgesics: may interfere with the pain transmission from periphery to center (cortex or thalamine). Some drugs alter the perception and response to pain
- Narcotic analgesics: these drugs alter the perception of pain experience and behavioral response to the pain
- Nonsteroidal anti-inflammatory drugs: may usually act at the periphery inhibiting the transmitting substance which cause pain
- Serotonin blockers: they act on serotonin by blocking its receptors. This analgesia is produced
- Anesthesia: the functional part of the nervous system is temporarily or permanently destroyed to interrupt pain transmission from periphery to the spinal cord and cerebral cortex or thalamus
- Nerve blocks: for this local anesthetics are used. The effect may be for few hours. Usually used before any short surgical procedures
Nursing management of pain:
Pain is considered as complex phenomena to understand and to assess as well. Pain has different components such as sensory, affective and cognitive
- Accept the patient as he is
- Accept and acknowledge the pain as what the patient feels or expresses
- Assist the individual to identify the situation when or where the pain started
- Assist the individual to identify the situation which intensifies the pain
- Do the assessment using the performa available
- Administer the drugs accordingly
- Give the individual to ventilate the feelings
- Give emotional support
- Give altered lifestyle to prevent situations which trigger the pain
- Family members can be involved in sessions
- Family members can be kept aware of the situation which can avoid the triggering of pain
- Family members can be taught some physical measures which can comfort the patient
- Most important nursing measure is to have a very good personal relationship to keep the patient physically and psychologically supported