ULTRASONOGRAPHY – Purpose, Preoperative Care, Post-Procedural Care and Potential Complications
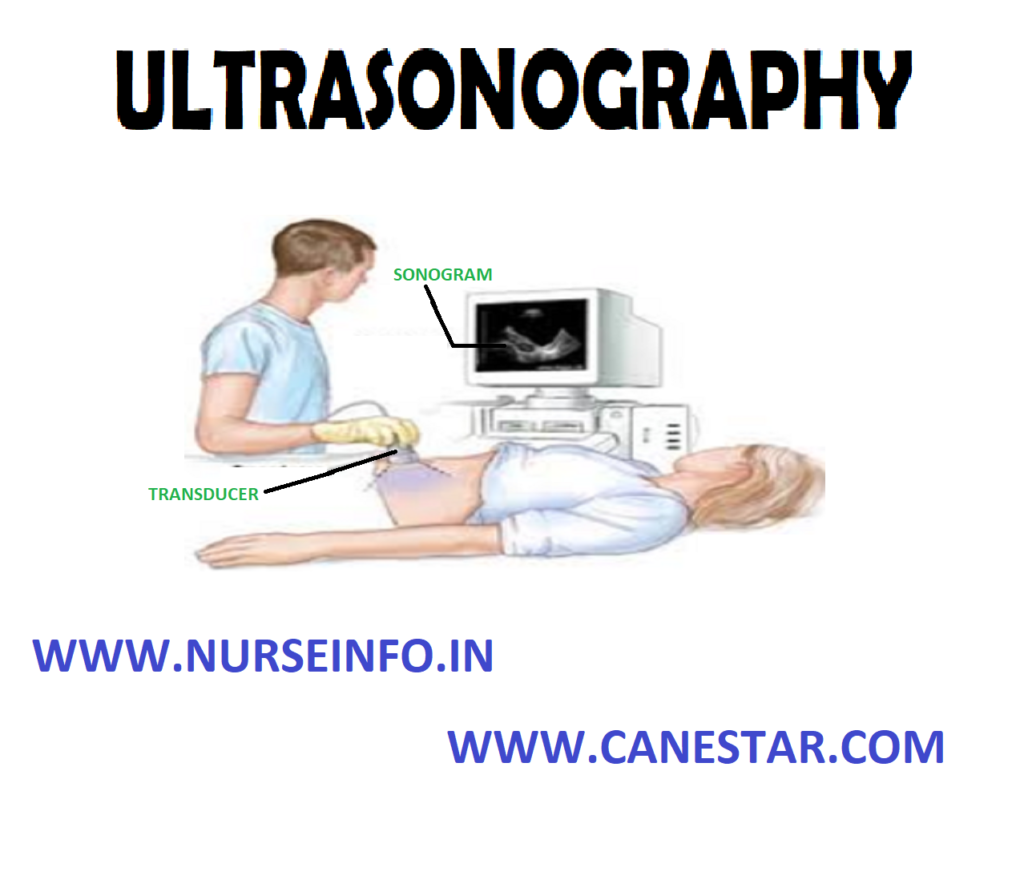
Ultrasonic waves (sound waves too high in frequency for a human ear or detect) are used diagnostically to assess various body structures. The waves are directed at the organ or structure, and as they vibrate back from the target, they are transducer into oscilloscope tracing.
Sonography may be used in conjunction with other pulmonary diagnostic procedures such as thoracentesis or pleural biopsy to assess fluid or fibrotic abnormalities
PURPOSE
- Ultrasonography is especially helpful and very accurate in detecting the amount and location of 50ml or less of pleural fluid. In comparison, a positive detection by chest radiography requires at least 500 ml of liquid
- If the technique is used in combination with thoracentesis, the ultrasonographer can determine the best location for the needle placement as well as the depth of the fluid
- Ultrasonography facilitates obtaining an adequate amount of fluid for laboratory analysis without unnecessary punching and probing
PREOPERATIVE CARE
- No special care is required before ultrasonography. Explain the purpose of the test and what to expect
- A gel is applied to the skin, a transducer (a device that changes reflected high-frequency sound to electrical energy) is moved on the skin surface above the target organ
- Inform the client that the procedure is painless and fairly quick
Procedure: a lung angiogram is administered by inserting a thin tube, or catheter into a vein leading to the lungs. This tube is then guided to the area that requires studying after which the iodine is injected in order to provide a contrasting color of the veins on the final X-ray. During the procedure, you are probably going to be asked to put on a lead gown to protect the genital and pelvic areas from X-ray exposure and a round cylinder or rectangular box that captures the images will be passed over the targeted area
- The clients are placed on an X-ray table in the supine position
- Electrocardiography electrodes are attached for cardiac monitoring
- The catheter is placed into the femoral vein and passed into the inferior vena cave
- With fluoroscopic visualization, the catheter is advanced to the right atrium and the right ventricle
- The catheter is manipulated into the main pulmonary artery, where the dye is injected
- X-ray films of the chest are immediately taken in timed sequence. This allows all vessels visualized by the injection to be photographed. If filling defects are seen in the contrast-filled vessels, pulmonary emboli are present
- If bronchial artery is performed, the femoral artery is cannulated instead of the vein
- During injection of dye, inform the client he or she will feel a burning sensation and flush throughout the body
POST-PROCEDURAL CARE
- Observe the catheter insertion site for inflammation, hemorrhage and hematoma
- Assess the client’s vital signs for evidence of bleeding (decreased blood pressure, increased pulse)
- Apply cold compress to puncture site if needed to reduce swelling or discomfort
- Inform the client that coughing may occur after this study
- Educate the client regarding the need for bed rest for 12 to 24 hours after the test
POTENTIAL COMPLICATIONS
- Allergic reaction to iodinated dye
- Hypoglycemia or acidosis may occur in clients who are taking metformin (glucophage) and receive iodine dye
- Cardiac arrhythmia: premature ventricular contractions during right-sided heart catheterization may lead to ventricular tachycardia and ventricular fibrillation
Contraindication: CT pulmonary angiogram (CTPA) is less desirable in pregnancy due to the amount of ionizing radiation required, which may damage the breasts, which are particularly sensitive during pregnancy, and because of concerns of the effects of iodine on the fetus’ thyroid gland. Nevertheless, CTPA is generally preferred to isotope studies in pregnancy, due to the lower radiation dose to the fetus.
Diagnostic algorithms for pulmonary embolism in pregnancy vary; however, a common compromise is to perform ultrasound testing for deep vein thrombosis of the legs, and if this is positive, make the diagnosis of pulmonary embolism on the basis of symptoms and presence of the DVT. CTPA would then only be performed if exhaustive non-radiation based testing could not make a positive diagnosis