RHEUMATOID ARTHRITIS – Etiology and Risk Factors, Pathophysiology, Clinical Manifestations, Diagnostic Evaluations and Management
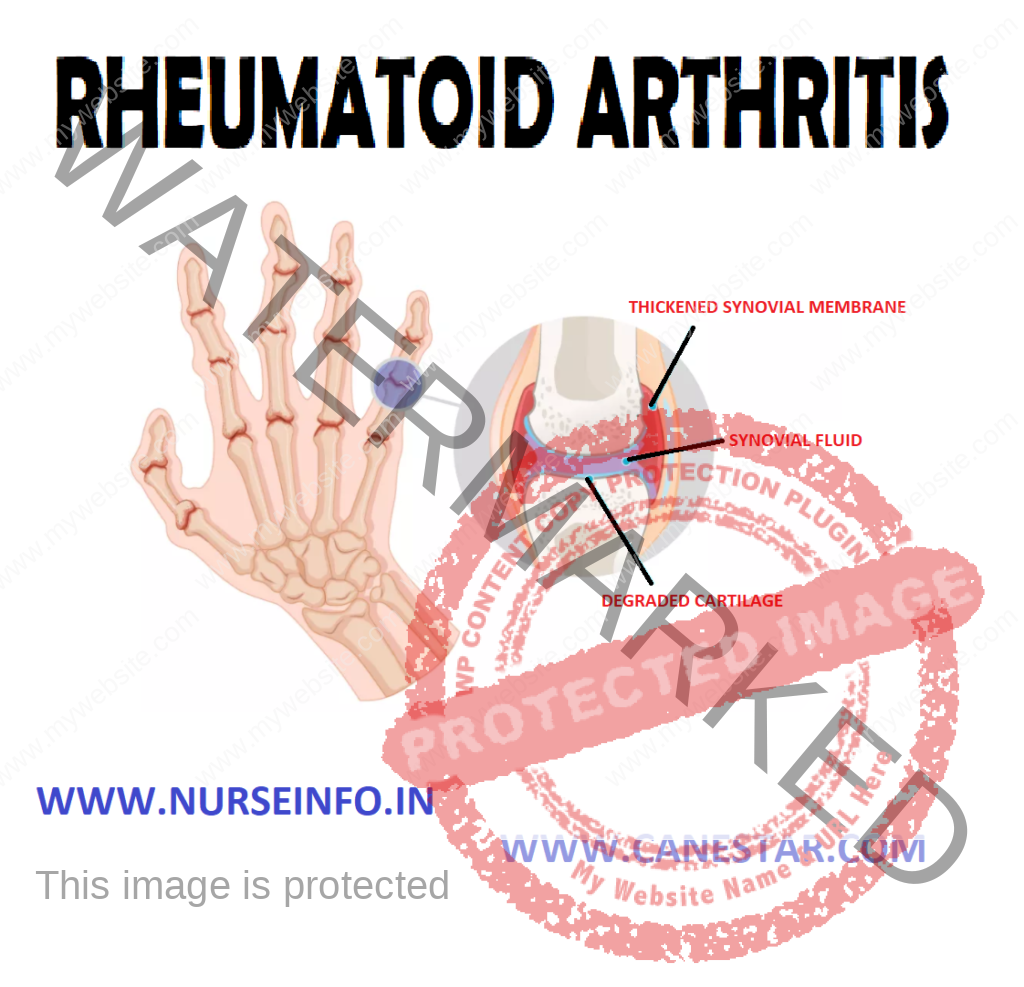
Rheumatoid arthritis is a chronic inflammatory disorder that typically affects the small joints in hands and feet.
It is an autoimmune disorder, it occurs when immune system mistakenly attacks own body’s tissues. In addition to causing joint problems, rheumatoid arthritis sometimes can affect other organs of the body – such as the skin, eyes, lungs and blood vessels.
ETIOLOGY AND RISK FACTORS
- The causes of rheumatoid arthritis are unknown
- It is believed that the tendency to develop rheumatoid arthritis may be genetically inherited (hereditary)
RISK FACTORS
- Age: risk increases with age
- Gender: women are more affected than men
- Genetic risk: there is a strong familial link in some cases
PATHOPHYSIOLOGY
Due to any cause —- synovitis —- increase in the lymphocytes and plasma cells —- articular cartilage destruction —- granulation tissue grows across the surface of cartilage (pannus) from the ending of joint —- articular surface shows loss of cartilage beneath the expanding pannus —- inflammatory pannus causes causes focal destruction of bones —- deformity and soft tissue swelling
CLINICAL MANIFESTATIONS
- Fatigue
- Anorexia
- Weight loss
- Stiffness
- Lack of appetite
- Low-grade fever
- Muscle and joint aches
Specific articular involvement is manifested
- Pain stiffness limitation of motion and signs of inflammation (heat swelling tenderness)
Extra-articular Manifestations
- Peripheral edema
- Peripheral neuropathy
- Myositis
- Tenocynovitis
- Rheumatoid vasculitis
- Sjorgen’s syndrome
- Amyloidosis
- Fetly syndrome
COMPLICATIONS
- Osteoporosis: rheumatoid arthritis itself, along with some medications used for treating rheumatoid arthritis, can increase the risk of osteoporosis – a condition that weakens bones and makes them more prone to fracture
- Carpal tunnel syndrome: if rheumatoid arthritis affects wrists, the inflammation can compress the nerve that serves most of hand and fingers
- Heart problems: rheumatoid arthritis can increase risk of hardened and blocked arteries, as well as inflammation of the sac that encloses heart
- Lung diseases: people with rheumatoid arthritis have an increased risk of inflammation and scarring of the lung tissues, which can lead to progressive shortness of breath
DIAGNOSTIC EVALUATION
- History collection
- Physical examination: check points for swelling, redness and warmth. Also check reflexes and muscle strength
- Laboratory tests
Complete blood count (CBC): people with rheumatoid arthritis tend to have an elevated erythrocyte sedimentation rate (ESR), which indicates the presence of an inflammatory process in the body.
- Radiographic studies of joint: X-rays help to track the progression of rheumatoid arthritis in your joints overtime
- Synovial fluid analysis
TREATMENT
- NSAIDs: are medications that can reduce tissue inflammation, pain, and swelling, e.g. brufen, etc
- Steroids: corticosteroids medications such as prednisone reduce inflammation and pain and slow joint damge
- Disease-modifying antirheumatic drugs (DMARDs): these drugs can slow the progression of rheumatoid arthritis and save the joints and other tissues from permanent damage. Common DMARDs include methotrexate, leflunomide, hydroxychloroquine and sulfasalazine
- Calcium and vitamin D supplements: to prevent thinning of the bones due to osteoporosis
Surgical Management
If medications fail to prevent or slow joint damage, surgery may help to restore ability to use joint
Rheumatoid arthritis surgery may involve one or more of the following procedures:
- Total joint replacement: during joint replacement surgery, surgeon removes the damaged parts of joint and inserts a prosthesis made of metal and plastic
- Tendon repair: inflammation and joint damage may cause tendons around joint to loosen or rupture. Repair the tendons around joint
- Joint fusion: surgically fusing a joint may be recommended to stabilize or realign a joint and for pain relief when a joint replacement is not an option
NURSING MANAGEMENT
Nursing Diagnosis
- Chronic pain related to joint inflammation and overuse
Interventions
- Perform a comprehensive assessment of pain to include location characteristics, onset, duration, frequency, severity
- Evaluate with patient and health care team, effectiveness of past pain control measures that have been used
- Reduce or eliminate the factors that increase the pain experience (e.g. fear fatigue lack of knowledge)
- Teach use of nonpharmacological techniques (relaxation, distraction, massage)
- Provide optimal pain relief with prescribed analgesics
- Impaired physical mobility related to joint pain and stiffness
Interventions
- Determine the limitations of joint movement and affect on function to establish baseline plan of care
- Collaborate with physical therapy into establish exercises program to improve the joint function
- Explain the plan and purpose of exercises to the patient and family
- Initiate pain control measures before beginning of joint exercises (hot packs, warm shower)
- Assist patient to do active, passive joint movements (selection of proper footwear use of assistive devices)
- Self-care deficit related to disease progression, weakness
Interventions
- Monitor patient’s ability for independent self care
- Monitor patients need for hygiene, dressing, grooming, eating
- Establish a routine for self-care activities assist patient in accepting dependency needs to ensure all needs are meet
- Teach family to encourage independence and to intervene only when patient is unable