UTERINE MASSAGE – Steps Involved in Uterine Massage and Expel Clots (MATERNAL AND CHILD HEALTH NURSING)
The rapid changes that the postpartum woman experiences can be expedited and supported with massage therapy. Massage can be given both immediately after birth, to encourage complete expulsion of the placenta; and on an ongoing basis to help ease backaches, stress, fatigue, headaches and postpartum depression
Effects of labor: immediately after the placenta is delivered, postpartum recovery begins. For the new mother, this is an intense and dramatic period of physical and emotional adjustment. In additional societies, it was common to support the pregnant, laboring and postpartum woman with massage. However, applications were most important during the postpartum recovery period, to ensure that all remnants of the placenta were expelled and to encourage uterine involution (the return of the uterus to its pre-pregnant shape and size)
Just after birth, the mother’s abdomen is flaccid and the skin is loose. Stretch marks will prevent the skin from regaining its pre-pregnant firmness. Her intestines, bladder and other organs may be displaced
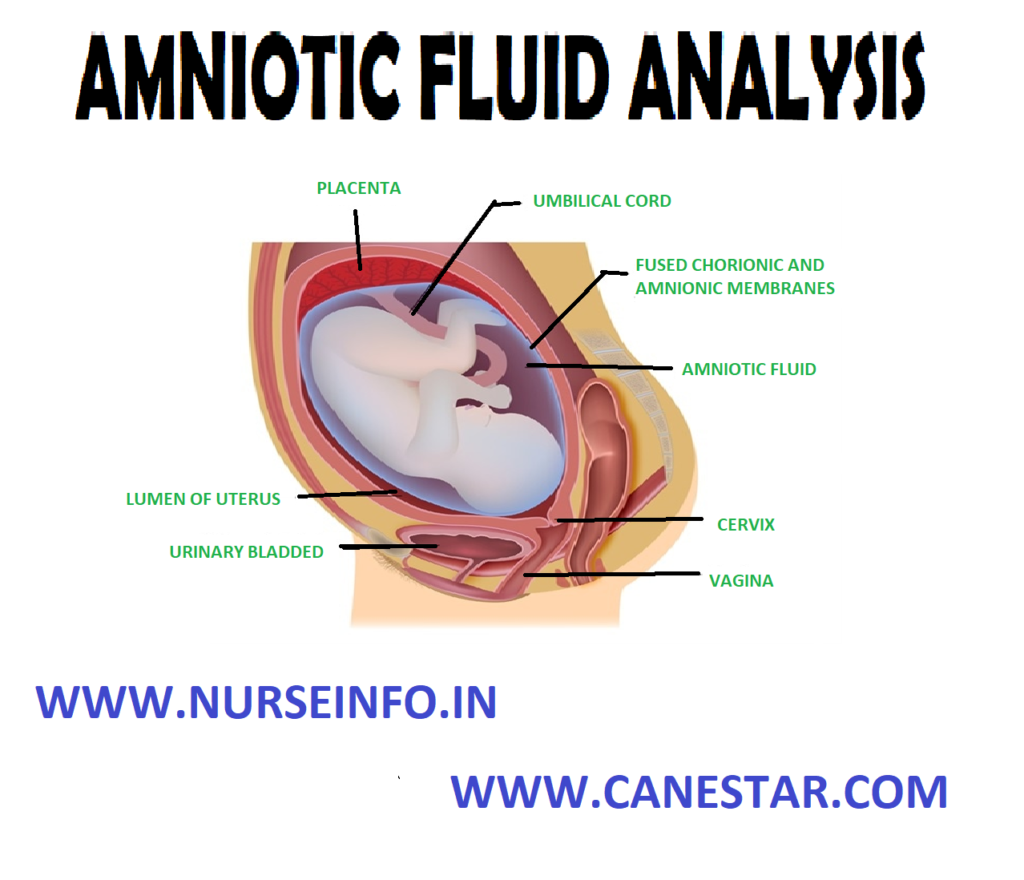
For several days after the birth of her baby, the new mother has an increase in urine output, hot flashes and heavy sweating, as her body rids itself of excess interstitial fluids and waste products. She will also lose anywhere from 10-12 pounds within hours of the birth, including 7-8 pounds of baby, 1-2 pounds of amniotic fluid and blood, and 1-2 pounds of placenta and other fluid
The uterus: after the placenta is delivered, the uterus continues to contract called “after pains”, these contractions are more common in women who have given birth before than in first-time mothers, and serve to restore the uterus to its prepregnant size and shape
Nursing mothers often complain about severe cramping because prolactin, the hormone of milk production, activates uterine contractions. These contractions serve an important purpose to expel any remaining clots and uterine tissue and control hemorrhages at the placental site
The day after the birth, the uterus is just above the umbilicus. Almost a week later, the top of the uterus is midway between the umbilicus and the symphysis pubis. After 10 days, the uterus has shrunk down behind the symphysis pubis
Abdominal massage immediately after the placenta is expelled can be painful, but it is very helpful in encouraging uterine involution and the flow of lochia, the natural postpartum discharge. The massage, which can be performed by the new mother on herself, is done on the abdomen in a clockwise direction using small, circular kneading strokes
The uterus should harden and contract with this treatment and the massage should be applied every four hours until the discharge is pale, for about 2-3 weeks. A woman who has had a cesarean (C-section) should take care to avoid direct pressure on her scar until it heals
STEPS INVOLVED IN UTERINE MASSAGE AND EXPEL CLOTS
- This should be carried out in case heavy postpartum bleeding persists after the placenta is delivered, or the uterus is not well-contracted (is soft)
- Place your cupped palm on the uterine fundus and feel for the state of contraction
- Massage the uterine fundus in a circular motion with the cupped palm until the uterus is well-contracted
- When well-contracted, place your fingers behind the fundus and push down in one swift action to expel clots
- Collect the blood in a container or over a clean plastic sheet placed close to the vulva. Estimate and record the amount of blood lost